BY ORDER OF THE
SECRETARY OF THE AIR FORCE
AIR FORCE INSTRUCTION 44-176
8 SEPTEMBER 2017
Certified Current 22 April 2020
Medical
A
CCESS TO CARE CONTINUUM
COMPLIANCE WITH THIS PUBLICATION IS MANDATORY
ACCESSIBILITY: Publications and forms are available on the e-Publishing website at
RELEASABILITY: There are no releasability restrictions on this publication.
OPR: AFMSA/SG3S
Supersedes: AFI44-176, 30 October 2014
Certified by: AF/SG3/5
(Maj Gen Roosevelt Allen Jr.)
Pages: 65
AFMS Access to Care Policy and Procedures
This publication implements AFPD 44-1, Medical Operations. It provides guidance and
procedures for Access to Care (ATC) operations within the Air Force Medical Service (AFMS).
It establishes the roles, responsibilities, definitions and requirements for implementing,
sustaining and managing ATC for AFMS Military Treatment Facilities (MTFs). Organizational
alignment of these functions may vary between MTFs. It applies to individuals at all levels
including the Air Force Reserve and Air National Guard (ANG), contract personnel and
volunteers who are working in military treatment facilities except where noted otherwise. This
publication may be supplemented at any level, but all supplements are routed to the Office of
Primary Responsibility (OPR) listed above for coordination prior to certification and approval.
Refer recommended changes and questions about this publication to the OPR listed above using
the AF Form 847, Recommendation for Change of Publication; route AF Forms 847 from the
field through the appropriate chain of command. The authorities to waive wing/unit level
requirements in this publication are identified with a Tier (“T-0, T-1, T-2, and T-3”) number
following the compliance statement. See AFI 33-360, Publications and Forms Management,
Table 1.1 for a description of the authorities associated with the Tier numbers. Submit requests
for waivers through the chain of command to the appropriate Tier waiver approval authority, or
alternately, to the Publication OPR for non-tiered compliance items. Ensure that all records
created as a result of processes prescribed in this publication are maintained IAW Air Force
Manual (AFMAN) 33-363, Management of Records, and disposed of IAW the Air Force
Records Disposition Schedule (RDS) in the Air Force Records Information Management System
(AFRIMS). Program Managers have a legally approved records disposition per the eGovernment
Act and National Archives and Records Administration (NARA) Bulletin 2010-02 that governs
2 AFI44-176 8 SEPTEMBER 2017
the data in approved IT systems/databases when no longer needed for the business of the Air
Force. The use of the name or mark of any specific manufacturer, commercial product,
commodity, or service in this publication does not imply endorsement by the Air Force.
SUMMARY OF CHANGES
This document has been substantially revised. This rewrite of AFI 44-176 includes: more
detailed roles and responsibilities to include GPM and TOPA Flight Commander; more closely
aligned with AFI 44-171, Patient Centered Medical Home Operations; addition of distinct
schedule, template and appointment management sections; inclusion of MHS GENESIS
Electronic Health Record (EHR) system; expansion of available schedules to 180 days in sync
with proposed MHS guidance; schedule guidance for Graduate Medical Education (GME)
residents and their preceptors; demand management and analysis guidance; changes in schedule
management and timeframes (to include the elimination of the use of dollar signs in appointment
types); inclusion of simplified appointing; first call resolution guidance; referral management;
changes in no-show guidance, changes in self-referral appointing instructions; inclusion of
consolidated specialty care management guidance; guidance for telephone administration;
detailed Nurse Advice Line (NAL) instructions; inclusion of TRICARE Online roles and
responsibilities. It is not directed toward dental clinics within the AFMS.
Chapter 1— PROGRAM OVERVIEW 6
1.1. Definition of Access To Care (ATC) Management. ............................................... 6
1.2. Goal of ATC Management...................................................................................... 6
1.3. Objectives of ATC Management. ........................................................................... 6
1.4. Health Insurance Portability and Accountability Act (HIPAA) Compliance. ........ 7
Chapter 2— ROLES AND RESPONSIBILITIES 8
2.1. The Military Treatment Facility (MTF) Commander will: ..................................... 8
2.2. The Access Manager/Access Management Team (AMT) will: .............................. 9
2.3. The Group Practice Manager (GPM) will: ............................................................. 9
2.4. The TOPA Flight Commander will: ....................................................................... 10
Chapter 3— SCHEDULE MANAGEMENT 11
3.1. Schedule Management. ........................................................................................... 11
3.2. Planning and Forecasting. ....................................................................................... 11
3.3. Implementation and Management. .......................................................................... 11
3.4. Analysis. ................................................................................................................. 12
AFI44-176 8 SEPTEMBER 2017 3
Chapter 4— TEMPLATE MANAGEMENT 13
4.1. Template Management............................................................................................ 13
4.2. Use of Detail Codes. ............................................................................................... 13
4.3. TRICARE Online (TOL) Web Enabled Detail Code. ............................................ 13
4.4. Provider Book Only (PBO) Detail Code. ............................................................... 13
4.5. Patient Access Type Detail Codes. ......................................................................... 13
Chapter 5— APPOINTING 14
5.1. Appointment Management...................................................................................... 14
5.2. Defense Enrollment Eligibility Reporting System (DEERS) Checks..................... 14
5.3. ATC Categories. ..................................................................................................... 14
Table 5.1. Military Health System (MHS) Standard Appointment Types. .............................. 15
5.4. Simplified Appointing. ........................................................................................... 15
Table 5.2. Appointment Measures. .......................................................................................... 16
5.5. Booking Transactions. ............................................................................................ 17
5.6. Continuity List Patients. ......................................................................................... 17
5.7. First Call Resolution. .............................................................................................. 17
5.8. Left Without Being Seen (LWOBS). ...................................................................... 18
5.9. No-Shows................................................................................................................ 18
5.10. Late Patient Arrival for Scheduled Appointment (Late-Show) .............................. 19
5.11. Patient Cancellations. .............................................................................................. 19
5.12. Facility Cancellations. ............................................................................................ 19
5.13. Appointing Data Quality/End of Day Processing. .................................................. 19
Chapter 6— APPOINTING INFORMATION SYSTEM OPERATIONS 21
6.1. Division, Clinic, and Provider Profiles. .................................................................. 21
6.2. Appointing Information System Booking Authority and Security Key
Administration. ........................................................................................................ 21
6.3. Telephonic/Text/Email Appointment Reminder Systems. ..................................... 21
Chapter 7— TELEPHONE ADMINISTRATION AND SUPPORT TO APPOINTING 22
7.1. Appointing Telephony Functional Responsibilities. ............................................... 22
4 AFI44-176 8 SEPTEMBER 2017
7.2. Telephonic Access Management Duties. ................................................................ 22
7.3. Automatic Call Distribution (ACD) Call Tree Considerations. .............................. 22
Chapter 8— NURSE ADVICE LINE 24
8.1. General. ................................................................................................................... 24
8.2. NAL Metrics. .......................................................................................................... 24
8.3. Roles and Responsibilities. ..................................................................................... 24
8.4. NAL Sustainment Guidance. .................................................................................. 26
8.5. Training. .................................................................................................................. 26
8.6. Guidance on Beneficiary Initiated Contact with MTF. ........................................... 26
8.7. Guidance on Warm Handoffs. ................................................................................ 26
8.8. CHCS and Application Virtualization Hosting Environment (AVHE) Guidance. . 27
8.9. Guidance on Clinic & MTF Closures. .................................................................... 27
8.10. Marketing Guidance. .............................................................................................. 27
Chapter 9— REFERRAL MANAGEMENT 28
9.1. General. ................................................................................................................... 28
9.2. Referring Provider Responsibilities. ....................................................................... 29
9.3. Specialist Responsibilities. ..................................................................................... 29
9.4. Referral Management Center (RMC) Responsibilities. .......................................... 29
Chapter 10— AIR RESERVE COMPONENT (ARC) ACCESS TO CARE 31
10.1. Introduction. ............................................................................................................ 31
10.2. ARC Health Care Benefits for Air Force Required Evaluations. ........................... 31
10.3. ARC Access to Care for Line of Duty (LOD) Determinations. .............................. 32
10.4. ARC Referrals. ........................................................................................................ 32
Chapter 11— SPECIALTY CARE 34
11.1. Overview. ................................................................................................................ 34
11.2. Schedule Planning and Forecasting. ....................................................................... 34
11.3. Schedule Implementation and Management. .......................................................... 34
11.4. Analysis. ................................................................................................................. 34
11.5. Mental Health ATC Management. .......................................................................... 34
AFI44-176 8 SEPTEMBER 2017 5
11.6. Physical Therapy (PT) Direct Access Management. .............................................. 36
11.7. Audiology/Hearing Conservation ........................................................................... 37
Chapter 12— ACCESS TEAM TRAINING, MANAGEMENT AND TRAINING
RESOURCES 38
12.1. Management and Training of GPMs: ..................................................................... 38
12.2. Training of Appointing Agents: .............................................................................. 38
Chapter 13— TRICARE ONLINE 39
13.1. TRICARE Online (TOL) Overview. ...................................................................... 39
13.2. TRICARE Online Roles and Responsibilities. ....................................................... 39
Attachment 1— GLOSSARY OF REFERENCES AND SUPPORTING INFORMATION 43
Attachment 2— AFMS REFERRAL MANAGEMENT (RM) BUSINESS RULES (BRS) 46
Attachment 3—(Added) ACCESS MANAGEMENT TEAM (AMT) AGENDA 65
6 AFI44-176 8 SEPTEMBER 2017
Chapter 1
PROGRAM OVERVIEW
1.1. Definition of Access To Care (ATC) Management. ATC management encompasses a
myriad of MTF functions and is an integral part of inpatient and outpatient, primary and
specialty healthcare delivery. ATC management includes, but is not limited to: day-to-day
management of templating, scheduling, and appointing functions, including appointments made
by telephone, in-person, electronic secure messaging, and web-based capabilities; information
systems management, including provider file and table building, and clinic/provider profile
management; empanelment, demand management and analysis; referral management activities;
appointing telephony management; and effective and efficient personnel management in support
of this mission. ATC also includes the concept of Enhanced Access which encompasses
healthcare management of the patient by the entire healthcare team through the use of clinical
support staff and non-traditional face-to-face physician/provider visits. Under Enhanced Access,
the healthcare team is expanded to include Clinical Pharmacists, Behavioral Health Optimization
Program (BHOP) providers, the Base Operational Medical Cell (BOMC), and Medical
Management (MM) personnel. Enhanced Access includes the use of Secure Messaging (SM),
the Nurse Advice Line (NAL), telemedicine, and direct access Physical Therapy (PT). Enhanced
Access will be incorporated into the MTF ATC strategy.
1.2. Goal of ATC Management. The goal of ATC management is to implement and sustain a
systematic, proactive, programmatic, and responsive access program for all clinics and services
across the MTF. MTFs must ensure appointment access meets the standards as stated in Title 32
Code of Federal Regulations 199.17, implemented by the Office of the Secretary of Defense
(OSD) in Department of Defense Instruction (DoDI) 6025.20 (Medical Management (MM)
Programs in the Direct Care System (DCS) and Remote Areas). The desired outcome is the
patient is provided the right healthcare service, at the right time, in the right setting within a
patient centric, not staff centric focus. The right setting may include over the phone, in the office,
or virtually, and it may be with a provider other than a physician. (T-0)
1.3. Objectives of ATC Management. The objectives of ATC management are to deliver
patient-centric access to services, meet mission requirements, and satisfy the wellness needs of
beneficiaries. Specifically, the AFMS’ access objectives are to:
1.3.1. Provide access to healthcare services/appointments within access standards.
1.3.2. Achieve patient and staff satisfaction.
1.3.3. Provide a patient-centered, first call resolution appointment system.
1.3.4. Implement Enhanced Access strategies.
1.3.5. Maximize patient-provider continuity.
1.3.6. Meet the healthcare needs of beneficiaries.
AFI44-176 8 SEPTEMBER 2017 7
1.4. Health Insurance Portability and Accountability Act (HIPAA) Compliance. MTFs
must ensure ATC Management functions comply with the HIPAA privacy and security programs
and national standards, including compliance with DOD 6025.18-R, DOD Health Information
Privacy Regulation, DOD 8580.02-R, DOD Health Information Security Regulation, or as
superseded by new or revised HIPAA privacy or security regulations and instructions. (T-0)
8 AFI44-176 8 SEPTEMBER 2017
Chapter 2
ROLES AND RESPONSIBILITIES
2.1. The Military Treatment Facility (MTF) Commander will:
2.1.1. Provide a supply of primary and specialty care appointments that meet patients’ total
demand for healthcare within ATC standards; mission and currency requirements; the
AFMS’ Strategy objectives and performance measures; and contain purchased care costs for
services available at the MTF. (T-1)
2.1.2. Set standards and procedures to maintain patient continuity with their Primary Care
Manager (PCM) in accordance with (IAW) AFI 44-171, Patient Centered Medical Home
Operations. (T-2)
2.1.3. Establish processes that enable follow up care and initial specialty care appointments
for new referrals to be appointed to the direct care system before the patient leaves the MTF.
Appointed means the patient has been booked with a time and place for future care. (T-1)
2.1.4. Ensure the MTF’s Capability and Capacity report is as unrestrictive as possible to
retain/recapture the maximum number of specialty care referrals to sustain clinical currency
and minimize purchased care costs. Retain authority for or assign an Executive Staff member
as the approval authority for changes to the MTF’s Capability and Capacity report. (T-1)
2.1.5. Provide “first call resolution” IAW paragraph 5.7 of this AFI at all central
appointment centers, RMCs and clinics that book primary care and initial specialty
appointments. (T-0)
2.1.6. Appoint the Group Practice Manager (GPM) as the Access Manager. (T-2)
2.1.7. Charter a multidisciplinary Access Management Team (AMT) to continuously
optimize the MTF’s patient-centric ATC strategy. (T-2)
2.1.8. Ensure ATC performance measures are briefed monthly at the Executive Committee
meeting. (T-2)
2.1.9. Publish and market the AFMS no-show standard, IAW paragraph 5.8 of this AFI, to
all MTF staff and beneficiaries and ensure it is applied throughout the MTF to enable a
consistent patient experience. (T-2)
2.1.10. Impress on their staff that the NAL is a DHA-run but Service-led operation which
enhances beneficiaries' access to care while giving the MTFs the opportunity to reduce
leakage to the network. The MTF will support the NAL in these efforts and will utilize all
available staff and resources to develop processes to support and promote NAL usage. (T-1)
2.1.11. Ensure MDG personnel are adequately trained to implement NAL processes and
initiatives IAW TRICARE NAL Operational Guidance. (T-1)
2.1.12. Establish processes to enhance and market the use of Secure Messaging, as well as
assign responsibility for Secure Messaging management.
2.1.13. Establish processes for the pre-approval of clinical staff to nonclinical positions, as
this will impact clinical capacity and capability. Ensure matrixing of clinical staff to
AFI44-176 8 SEPTEMBER 2017 9
nonclinical positions is kept to a minimum, except for where an adverse action exists per AFI
44-119, Medical Quality Operations.
2.2. The Access Manager/Access Management Team (AMT) will:
2.2.1. Be chaired by the GPM. The Chief of the Medical Staff (SGH) will be the alternate
chair. The AMT will follow the agenda outlined in Attachment 3 of AFI 44-176. (T-2)
2.2.2. Include at a minimum: the Access Manager, all GPMs, SGH, Chief Nurse (SGN);
Administrator (SGA); Health Care Integrator (HCI); Health Service Management 4A
Functional or representative; Aerospace Medicine Chief (SGP) or representative; Flight
Commanders of all clinics, TRICARE Operations and Patient Administration (TOPA) Flight
Commander, the Quality Manager, and the lead appointment agent. (T-2)
2.2.2.1. The Medical Operations Squadron (MDOS), Medical Support Squadron
(MDSS) and Aerospace Medicine Squadron (AMDS), and Surgical Operations Squadron
(SGCS) Commanders are highly encouraged to participate and/or be members of the
AMT.
2.2.3. Meet in-person with AMT members listed in para 2.2.2 above at least monthly to
review/coordinate templating, scheduling, appointing, clinic/appointment staffing, provider
coverage, supply shortfalls and surpluses, and other clinical operational issues with the goal
of optimizing ATC at the MTF. The AMT will discuss process improvement efforts. (T-2)
2.2.4. Review performance measures for all clinics monthly, to include but not limited to:
Third Next available appointment (24HR, FTR, SPEC), appointment utilization, demand
management purchased care leakage, patient satisfaction, telephony metrics, no-show
metrics, first call resolution results, PCM continuity measures, and NAL metrics. (T-2) See
Attachment 3 for full list of measures to be reviewed at the AMT.
2.2.5. Document evidence of meeting occurrence (i.e. slides and sign-in roster). Formal
meeting minutes are encouraged but not required. (T-2)
2.2.6. The AMT will review the Nurse Advice Line (NAL) sustainment plan annually. (T-2)
2.3. The Group Practice Manager (GPM) will:
2.3.1. Chair the AMT. (T-2)
2.3.2. Recommend access improvement strategies and at minimum report deficient access-
related performance measures/results to the Executive Committee at least monthly through
the AMT in accordance with paragraph 2.2.4 above. (T-2)
2.3.3. Monitor/analyze NAL appointment booking, usage and performance metrics. (T-2)
2.3.4. Perform continuous demand management forecasting. (T-2)
2.3.5. Develop and modify provider templates. (T-3) This should be done in conjunction
with providers and clinic leadership (e.g. Flight Commander/Flight Chief, etc.).
2.3.6. Collaborate with providers and clinic leadership to provide an adequate supply of
appointments through management of templates, schedules, appointing procedures and
utilization of access enhancing tools. (T-2)
10 AFI44-176 8 SEPTEMBER 2017
2.3.7. Develop processes to ensure that appointment templates and appointing protocols are
reviewed and approved no less than semi-annually by providers, Flight Commanders, SGH
and appropriate SQ/CC. (T-3)
2.3.8. Provide current booking protocols to appointing staff and review protocols quarterly.
(T-3)
2.3.9. Be involved in MTF business plan development and execution. (T-3)
2.3.10. Provide the number of administratively closed (ADMIN) appointments performed in
Composite Health Care System (CHCS) or MHS GENESIS to the Data Quality Team. (T-3)
2.3.11. Coordinate with the Health Care Integrator (HCI) and SGH to determine appropriate
provider empanelments. (T-3)
2.3.12. The GPM will analyze unfilled appointments to determine the root causes of non-use
through the use of available ATC Tools such as the TRICARE Operations Center (TOC) and
Direct Access Reporting Tool (DART). (T-2) The MTF should consider factors such as type
of appointment, time appointment offered, purchased care leakage for the same services,
detail codes restrictions, etc.
2.3.13. The GPM will analyze published schedules to determine the effectiveness of meeting
patient demand relative to the quantity of appointments: time of available appointments,
over/under supply of appointment mix, seasonality impacts, cancellations, no-shows,
schedule changes, etc. (T-3)
2.3.14. The GPM will follow responsibilities as outlined in Chapter 7 and Chapter 11 of
this document. (T-3)
2.3.15. The GPM will attend required events as outlined in Chapter 12 of this document.
(T-3)
2.4. The TOPA Flight Commander will:
2.4.1. Manage the Referral Management Center (RMC) to ensure the requirements as
outlined in Chapter 8 and Appendix 2 of this document are met. (T-3)
2.4.2. Complete Referral Management (RM) related Management Internal Control Toolset
(MICT) checklist IAW MICT guidance criteria pertaining to this AFI. This can also be
completed by TOPA personnel appointed by the TOPA Flight Commander. (T-3)
2.4.3. Be the primary Functional Requirements Evaluator Designee (FRED) for the Air
Force Medical Support Agency (AFMSA) RMC central contract (only for participating
MTFs). The TOPA Flight Commander will assign an alternate FRED in writing. (T-3)
2.4.4. Manage the processing of patient enrollment and PCM empanelment/reassignment
within the electronic scheduling system (CHCS or MHS GENESIS). (T-3)
AFI44-176 8 SEPTEMBER 2017 11
Chapter 3
SCHEDULE MANAGEMENT
3.1. Schedule Management.
3.1.1. Schedule management encompasses continuous planning, forecasting,
implementation, management and analysis of provider and clinical staff schedules to meet
patient demand.
3.2. Planning and Forecasting.
3.2.1. The MTF will maintain a rolling 180-day schedule to ensure adequate provider and
clinic staff availability to meet patient demand within access standards. (T-0) Consider the
following in schedule development: historical patient utilization patterns, leave, TDY, base
exercises, down days, etc.
3.2.2. The AMT will analyze patient demand utilizing the measures listed in para 2.2.4
above and others as needed. (T-2) Effective management of appointments will maximize
patient access to the MTF and avoid purchased care leakage.
3.3. Implementation and Management.
3.3.1. Primary and specialty care clinics will provide a minimum of 180-calendar days of
available appointments for booking at all times. (T-0)
3.3.1.1. Graduate Medical Education (GME) residents and their preceptors will provide a
minimum of 60-calendar days of available appointments for booking at all times. (T-0)
3.3.1.2. Primary and specialty clinics shall not use the dollar sign appointment types. (T-
1) Use of dollar sign appointment types prevents the appointment from being booked,
thus limiting patient access to care.
3.3.2. The Template Manager (TM) will have written processes for appointment schedule
change requests with the goal of minimizing frequent/repeated changes to opened schedules,
changes causing facility cancellations, rescheduling of patients, etc. (T-3) This process
should be automated, as functionality to auto-reconfigure appointments exists in CHCS.
3.3.3. Primary Care clinics will convert unbooked FTR appointments to 24HR appointments
no later than (NLT) 24 hours prior to the scheduled appointment time. (T-2)
3.3.4. The TM will release/delete unbookable appointments (FROZ, WAIT, HOLD, etc.)
NLT 48 hours prior to the clinic day in which the unbookable appointments were scheduled.
(T-2) Appointments will be set up to auto-reconfigure.
3.3.5. The TM will not delete unbooked or unused appointment slots from the appointing
system. (T-1)
3.3.6. The TM will review the next clinic day’s appointment availability and mix daily to
ensure schedules meet patient demand and are adjusted as needed. (T-2)
12 AFI44-176 8 SEPTEMBER 2017
3.4. Analysis.
3.4.1. The GPM will analyze unfilled appointments to determine the root causes of non-use
through the use of available ATC Tools such as the TRICARE Operations Center (TOC) and
Direct Access Reporting Tool (DART). (T-3) The MTF should consider factors such as type
of appointment, time appointment offered, purchased care leakage for the same services,
detail codes restrictions, etc.
3.4.2. The GPM will analyze published schedules to determine the effectiveness of meeting
patient demand relative to the quantity of appointments: time of available appointments,
over/under supply of appointment mix, seasonality impacts, cancellations, no-shows,
schedule changes, etc. (T-3) This includes those clinics that offer sick call appointments.
AFI44-176 8 SEPTEMBER 2017 13
Chapter 4
TEMPLATE MANAGEMENT
4.1. Template Management.
4.1.1. MTFs will construct templates and schedules using the MHS Standard Appointment
types (see Table 5.1). Definitions can be found on the AFMS Knowledge Exchange (Kx)
ATC page. MTFs using MHS GENESIS will follow appointing procedures for MHS
GENESIS.
4.1.2. Primary care provider templates will be created IAW AFI 44-171 and will meet
forecasted patient demand for healthcare access. (T-2)
4.2. Use of Detail Codes.
4.2.1. MTFs may use detail codes to further define appointment types on templates and
schedules, IAW approved detail code list in MHS Guide for Access Success.
4.2.2. MTFs will use the tri-service approved operational definitions of detail codes. (T-2)
4.3. TRICARE Online (TOL) Web Enabled Detail Code.
4.3.1. Appointments, by default, are web enabled. MTFs will ensure at least 80 percent of
appointments in Family Health, Pediatrics, Internal Medicine, Flight Medicine Primary Care
clinics and Optometry clinics are web enabled. (T-0)
4.4. Provider Book Only (PBO) Detail Code.
4.4.1. In Primary Care clinics, the MTF will limit the use of the PBO detail code to those
appointments in excess of required centrally bookable appointment levels for AFMH, IAW
AFI 44-171. (T-2)
4.4.2. For initial specialty care referral appointments, the MTF will not use the PBO detail
code. (T-2)
4.5. Patient Access Type Detail Codes.
4.5.1. MTFs will use no more than two patient access type detail codes per appointment slot.
(T-3) This ensures appointing personnel correctly identify the eligible beneficiary category of
patient per TRICARE policy to be booked into a particular slot. (T-1)
14 AFI44-176 8 SEPTEMBER 2017
Chapter 5
APPOINTING
5.1. Appointment Management.
5.1.1. The MTF medical clinics will use the MHS electronic patient scheduling appointment
system to schedule patient appointments. (T-1)
5.1.2. MTF will provide equal priority access for TRICARE Prime beneficiaries not enrolled
to the MTF as for those enrolled to the MTF, US Family Health Plan enrollees may be seen
on a space available basis, IAW 32 CFR Sec. 199.17. (T-0) Prioritize according to Title 32
CFR 199.17 (d)(1) and Health Affairs Policy 11-005: Active Duty Family Members
(ADFMs) in Prime have priority access, followed by Retirees, etc.
5.1.3. The MTF staff who book patient appointments will match the patient’s request for
care with the appropriate ATC category. (T-0)
5.2. Defense Enrollment Eligibility Reporting System (DEERS) Checks.
5.2.1. The MTF staff will complete a DEERS eligibility check and patient demographic
information verification (current address and current telephone number) at each patient
interface (e.g., booking via telephone or in person, telephone consultation requests, and
check-in by a patient for any appointments, etc.). The only exception is for telephone
contacts made by/to providers. (T-0)
5.2.2. Patient eligibility for care and enrollment status should be addressed by TOPA IAW
AFI 41-210, TRICARE Operations and Patient Administration Functions.
5.3. ATC Categories.
5.3.1. Appointing personnel will select one of the ATC categories (see Table 5.1) in the
CHCS appointing search function in order to book scheduled appointments. (T-1) The
appropriate ATC standard is based on the timeline of the patient’s request for care or
provider directive. MTFs using MHS GENESIS will follow appointing procedures for MHS
GENESIS.
AFI44-176 8 SEPTEMBER 2017 15
Table 5.1. Military Health System (MHS) Standard Appointment Types.
MHS Standard
Appointment
Type
Timeline of Patient’s Request for Care (ATC
Standard)
ATC Category/
CHCS Search
Options
24HR
24 Continuous Hours/1440 minutes
Acute
WELL
28 Calendar Days/40,320 minutes
Wellness
SPEC
PROC
28 Calendar Days/40,320 minutes, or per Provider
Designation not to exceed 28 Calendar days
Specialty
FTR
GRP
No Standard or per Provider Designation
Future
5.4. Simplified Appointing.
5.4.1. All Primary Care clinics using the BAA, BDA, BDB, BGA and BJA Medical Expense
and Performance Reporting System (MEPRS) codes will utilize the Simplified Appointing
model in provider schedules. The 24HR, FTR, SPEC, PROC and GRP appointment types
will be used as described below. (T-0)
5.4.2. For most MTFs, a Primary Care schedule with a minimum of 50/50 mix of 24HR and
FTR appointments provides optimal access to meet patient demand. MTFs should utilize
demand management forecasting and available demand forecasting tools such as the Direct
Access Reporting Tool (DART) to determine the appropriate mix of appointments and to
adjust schedules as needed to provide a patient-centric supply of appointments.
5.4.3. Group Practice Managers will maximize the use of the 24HR and FTR appointment
types in Primary Care templates and schedules. (T-0) Only SPEC, PROC and GRP
appointment types may be added to the schedule to support provider practice patterns.
However, use of these appointment types should be consistent with AFI 44-171 bookable
appointments requirements and be complementary to maximize 24HR and FTR access to
care.
5.4.4. Definitions of Simplified Appointing Appointment Types.
5.4.4.1. 24HR: primarily used for patient care conditions requiring care within 24 hours
of the request. It may also be used for non-urgent patient conditions, but must be
balanced with urgency and availability; this process will be described in the MTF
appointing protocols. To the greatest extent possible, appointing staff will fill all open
24HR slots on a daily basis. Appointments will not be limited to “one complaint” or
medical issue, but rather will address all patient concerns that can be adequately covered
in the time allotted to minimize the need for unnecessary future appointments or repeat
visits.
16 AFI44-176 8 SEPTEMBER 2017
5.4.4.2. FTR: used for patients requesting non-urgent services beyond 24 hours (such as
for routine, wellness and follow-up care). The FTR appointment type will not be used for
initial specialty (SPEC) appointments. To the greatest extent possible, appointments will
not be limited to “one complaint” or medical issue, but rather will address all patient
concerns that can be adequately covered in the time allotted to minimize the need for
unnecessary future appointments or repeat visits.
5.4.4.3. SPEC: used for an initial consult/referral appointment. It may also be used for a
patient initiated self-referral appointment. The CHCS appointing system will
automatically assign the ATC Standard and Category that matches the referral’s clinical
priority entered by the requesting provider.
5.4.4.4. PROC: used for patients in need of medical procedures. A procedure
appointment will be booked and seen with a provider within 28 calendar days or per the
provider's designation. Within Primary Care clinics, a referral is generally not required. If
the PROC appointment is not performed within the patient’s medical home, a referral will
be required.
5.4.4.5. GRP: used for patients who require therapy, counseling, or teaching encounters
where a provider will perform the service in a group setting. The detail code fields can be
used to provide further information about the care to be provided in the group
appointment, (e.g., TOBCES for a Tobacco Cessation Class). A group appointment may
be scheduled per self-referral of the patient, or the clinic's or referring provider's policy or
designation.
5.4.5. Measurement. The following strategic measures will be utilized to measure the
success of Simplified Appointing (T-1):
Table 5.2. Appointment Measures.
Measure
Target
Report Location
Prospective Measures
3
RD
Available 24HR Appointment
≤ 1.0 days
TRICARE Operations
Center (TOC), Third
Available Report
Monthly
3
RD
Available FTR Appointment
3
RD
Available SPEC Appointment
3
RD
Available WELL Appointment
≤ 7.0 days
≤ 28.0 days
≤ 28.0 days
TOC, Third Available
Report Monthly
TOC, Third Available
Report Monthly
TOC, Third Available
Report Monthly
AFI44-176 8 SEPTEMBER 2017 17
Retrospective Measures
Average Days to Be Seen (Acute
search)
≤ 1.0 days
TOC, Access to Care
Summary Report
Average Days to Be Seen (Future
search)
≤ 14.0 days
TOC, Access to Care
Summary Report
5.5. Booking Transactions.
5.5.1. MTFs will use the access category search that best represents the patient's request. (T-
0)
5.5.2. MTFs will waive ATC standards should patients request appointments outside of ATC
standards for provider continuity/convenience/personal reasons, even though the MTF may
have appointments available inside ATC Standards with their PCM or other providers in the
team/clinic. (T-1) MTFs will not use ‘Just Looking’ feature in CHCS to search for
appointments.
5.5.3. Patients Refusing All Appointment Times Offered. Appointing personnel will
document patient refusals in CHCS, IAW current CHCS information system processes to
ensure it reflects the reason a patient refused all appointment times offered as opposed to
accepting an appointment within ATC standards. (T-3)
5.5.4. Unbooked Appointment Request Functionality. Appointing personnel will choose the
most accurate Unbooked Appointment Request as defined in the current MHS access to care
guide. (T-3)
5.6. Continuity List Patients.
5.6.1. Continuity List (CL) patients are those high-acuity patients who must be seen by their
provider due to the risk in both outcome, and/or unnecessary deferral to the network.
5.6.2. PCM Teams in Primary Care will develop and maintain a current list of their
continuity patients IAW AFI 44-171.
5.6.3. Patients identified as CL patients will be identified by [CL] in the remarks field of
CHCS. These patients will be offered a continuity appointment as outlined in AFI 44-171.
5.7. First Call Resolution.
5.7.1. MTFs will not divert patients to the NAL during business hours as a means to
complete first call resolution. (T-1)
5.7.2. Appointing agents will:
5.7.2.1. Search for appointments with the patient's PCM. If no appointments are
available, the agent will search within the PCM Team, then PCM Clinic, then across all
Primary Care clinics (this includes cross-booking into the following MEPRS: BAA -
Internal Medicine, BDA - Pediatrics, BGA- Family Health, BJA – Flight Medicine). (T-
1)

18 AFI44-176 8 SEPTEMBER 2017
5.7.2.2. If unable to find an appropriate appointment for the patient, transfer the call to
the patient's PCM team nurse or a designated clinic triage nurse, via warm hand-off, for
triage and appropriate disposition. (T-1)
5.7.2.3. If unable to warm-handoff the patient to the PCM team nurse, enter a high
priority T-CON (red in AHLTA) to the team indicating the need for a two-hour response.
(T-1)
5.7.3. PCM Team nurses will:
5.7.3.1. Take warm hand-off calls from appointing agents and determine the most
appropriate disposition. (T-1)
5.7.3.2. When warm hand-offs are not possible, reply to RED TCONs within two hours.
(T-1)
5.7.3.3. Ensure Active Duty patients are deferred to the network only as a last resort. (T-
1)
5.7.3.4. MTFs will use the Un-booked Appointment Request/Reporting functionality in
CHCS to allow for the tracking and reporting of patients who requested an appointment,
a search was performed by an appointing agent, but the appointment request did not
result in a booked appointment. (T-3)
5.8. Left Without Being Seen (LWOBS).
5.8.1. A patient who has a booked appointment, arrives at the clinic, and is checked in, but
leaves without seeing the provider.
5.9. No-Shows.
5.9.1. The MTF will designate an appointment a no-show when a patient does not keep a
scheduled appointment or cancels within 2 business hours of the appointment. Commanders
will publish and market the AFMS no-show standard to all MTF staff and beneficiaries and
ensure it is applied throughout the MTF to enable a consistent patient experience. (T-3) If a
patient is designated a no-show by cancelling within 2 business hours of the appointment,
every effort will be made to utilize the now unfilled appointment.
5.9.1.1. An individual clinic’s no-show rate will not exceed five (5) percent of all booked
appointments. (T-1) Specialty care clinics no-show rates will be IAW Chapter 11,
Specialty Care.
5.9.1.2. The MTF will use the following formula to calculate the no-show percentage
(T-1):
# No-Shows
(LWOBS + Kept + No Show + Pending)* – (Facility Cancelled + Patient Cancelled)
*all booked appointments
5.9.1.3. Providers, clinical staff and appointment line staff will attempt to contact (e.g.
voicemail, secure messaging, written letters, etc.) no-show and Left Without Being Seen
(LWOBS) patients at least once to ensure patient wellness/safety. All attempts will be
documented in the Electronic Health Record (EHR). (T-3)
AFI44-176 8 SEPTEMBER 2017 19
5.10. Late Patient Arrival for Scheduled Appointment (Late-Show) .
5.10.1. MTF Commanders will publish and market a single late-show policy to all MTF staff
and beneficiaries, and will ensure it is applied throughout the MTF to enable a consistent
patient experience. (T-3) Patients who arrive at the clinic greater than 10 minutes after their
scheduled appointment time are considered late. Every effort will be made to accommodate
late showed patients.
5.11. Patient Cancellations.
5.11.1. MTFs will establish a separate cancellation telephone number/call tree option that is
available/open 24 hours a day, seven days a week to capture patients’ appointment
cancellation requests. (T-3) The phone number will be clearly published on MTF websites,
appointment line messages, phone books and other communications. TRICARE Online
(TOL), Secure Messaging, and e-mail appointment cancellation notifications do not fulfill
this requirement.
5.11.2. MTFs will develop an ongoing process in which cancellations (via automated
appointment reminder, secure message, etc) are translated back into the appointing
information system thus, making cancelled appointments available for booking. (T-3)
5.12. Facility Cancellations.
5.12.1. MTFs will establish processes to minimize facility cancellations. (T-3)
5.12.2. MTFs will establish schedule management processes to govern the facility
cancellation process to include: approval authority; conditions when facility cancellation is
allowed (e.g., emergency weather conditions); and reporting and tracking of occurrences to
the MTF AMT. (T-3) Mental Health patients who are on the High Interest List (and are
therefore at elevated risk for harm or behavioral issues) are required to speak with a provider
prior to cancelling an appointment IAW AFI 44-172, Mental Health. (T-1)
5.12.3. MTFs shall notify affected patients of their facility cancelled appointment within one
business day of the facility cancellation. One business day includes the facility cancellation
date plus the end of the next business day. (T-3)
5.12.4. MTFs’ facility cancellation rate shall not exceed three percent of all booked
appointments. MTFs will use the below formula to calculate the facility cancellation rate:
(T-2)
# Facility Cancelled
_____________________________________________________
(LWOBS + Kept + Facility Cancelled + No shows + Pending)*
*number of patients who were booked appointments
5.13. Appointing Data Quality/End of Day Processing.
5.13.1. At the end of each business day, clinics will complete CHCS end of day processing.
(T-3)
5.13.2. Clinic staff will:
5.13.2.1. Determine and assign a patient appointment status for each appointment. (T-3)
20 AFI44-176 8 SEPTEMBER 2017
5.13.2.2. Process and apply workload types (count/non-count) on appointment slots to
match the actual care provided. (T-3)
5.13.2.3. Match the provider who actually saw the patient to the final appointment status.
(T-3)
5.13.2.4. Preserve Walk-in and Sick Call appointment statuses and will not change them
to any other appointment status. (T-3)
5.13.2.5. Preserve open/unused appointment slots and will not delete them from the
schedule. (T-3)
AFI44-176 8 SEPTEMBER 2017 21
Chapter 6
APPOINTING INFORMATION SYSTEM OPERATIONS
6.1. Division, Clinic, and Provider Profiles.
6.1.1. Executive staff will identify staff responsible to establish and maintain division, clinic
and provider profiles in CHCS. MTFs using MHS GENESIS will follow procedures for
MHS GENESIS. (T-3)
6.1.2. Executive staff will ensure the following settings in CHCS: (T-1)
6.1.2.1. Set the ATC Reporting Flag to "Yes" in each of its primary and
specialty/surgical care clinic profiles that have active schedules.
6.1.2.2. Set the Self-Referral flag to "Yes" in the clinic profile of primary care clinics to
accommodate cross-booking per AFI 44-171.
6.1.2.3. Set the Self-Referral flag to "Yes" in the clinic profile of the following specialty
care clinics: women’s health, nutritional medicine, optometry and mental health.
6.2. Appointing Information System Booking Authority and Security Key Administration.
6.2.1. Executive staff and GPM will establish who will have authority to book and cancel
appointments in the appointing information system which will be reviewed annually. (T-3)
6.2.2. Executive staff and GPM will identify positions and what appointment information
systems security keys are needed to perform required duties (T-3). These appointment
information system security keys include:
6.2.2.1. Changing appointment types.
6.2.2.2. Changing and/or adding detail codes.
6.2.2.3. Changing gender and age designations on appointment slots.
6.2.2.4. Booking appointments outside ATC standards.
6.2.2.5. Instantaneously creating/booking appointments while appointing the patient.
6.2.2.6. Deleting appointment slots.
6.2.2.7. Freezing and unfreezing appointment slots.
6.2.2.8. Facility canceling appointments.
6.3. Telephonic/Text/Email Appointment Reminder Systems.
6.3.1. Executive staff will identify at least two MTF personnel who are responsible and
trained to set up and maintain the appointment reminder systems (e.g., Audiocare, TOL,
Televox). (T-3) The executive staff will ensure that a local contingency plan is developed
and in place in the case there is a phone outage or other event that challenges
communications to and from the MTF.
6.3.1.1. MTF leadership will ensure that a local MTF marketing campaign is developed
to enroll patients in TOL or the current web-based telephonic/text/email reminder system.
(T-3)
22 AFI44-176 8 SEPTEMBER 2017
Chapter 7
TELEPHONE ADMINISTRATION AND SUPPORT TO APPOINTING
7.1. Appointing Telephony Functional Responsibilities.
7.1.1. The GPM will have primary functional control, and whenever possible, administrative
control of appointing personnel (telephone as well as front desk appointing). (T-2)
7.1.2. The GPM will monitor four (4) calls per month, per agent, and provide feedback on at
least two of those calls using the AFMSA/SG3S recommended quality monitoring scorecard.
(T-3)
7.1.3. Calls routed through the Automatic Call Distribution (ACD) may be recorded IAW
local labor laws, and may be retained for up to 30 days.
7.1.4. MTFs will select their ACD system after receiving approval from AFMSA/SG3S. (T-
1)
7.2. Telephonic Access Management Duties.
7.2.1. Key Performance Indicator (KPIs) targets that Telephonic Access Management
personnel will review are:
7.2.1.1. Percent of Abandoned Calls - Less than or Equal to 8%. (T-2)
7.2.1.2. Service Level – 90% of Calls Answered within 90 seconds. (T-2)
7.2.1.3. Average Speed of Answer – Less than or Equal to 45 seconds. (T-2)
7.2.1.4. Average Talk Time – Less than or equal to 180 seconds. (T-2)
7.2.2. The GPM is responsible for reporting KPI measurement outcomes to the Executive
Committee on a monthly basis and recommends improvement strategies through the AMT as
needed. (T-2)
7.3. Automatic Call Distribution (ACD) Call Tree Considerations.
7.3.1. The GPM and Telephonic Access Management personnel will ensure call trees will
not exceed five options in any given menu. (T-1) Not included in the five options are
cancelling an appointment, an option to return a caller to Option #1 on the menu, and an
option to repeat a menu.
7.3.2. The GPM and Telephonic Access Management personnel will ensure call menus do
not exceed six layers. (T-1)
7.3.3. Option #1 from the opening or main menu is to access the appointment desk/call
center function to book appointments at the MTF only. The GPM will ensure the Nurse
Advice Line (NAL) will not be made any part or sub-menus of Option #1. (T-1)
7.3.3.1. The GPM will ensure the NAL will be placed on the call tree as an option other
than Option #1 when the appointment line/call center is open for normal business hours
(i.e. Option #2 or #3 behind primary care, specialty care and dental appointments for the
MTF). (T-1) When the appointment line is closed, the NAL will be moved to Option #1.
(T-1)
AFI44-176 8 SEPTEMBER 2017 23
7.3.4. Each system will ensure any on-hold music represents a professional atmosphere and
is legally obtained for rebroadcast. (T-2)
7.3.5. The GPM will ensure skill set naming conventions start with the MEPRS code, to
ensure consistent data collection across the AFMS. (T-3)
7.3.6. All MTF PCM booked appointments are routed through the ACD to capture workload.
While the use of skill sets is encouraged for high volume clinics, the calls may be routed by
the ACD to a direct clinic line.
7.3.7. All changes to the call tree that impact the collection of ACD metrics must be
approved by the AFMSA/SG3S, Access To Care Program Office prior to implementation.
(T-1)
24 AFI44-176 8 SEPTEMBER 2017
Chapter 8
NURSE ADVICE LINE
8.1. General.
8.1.1. Military Treatment Facilities (MTF) will establish a written Nurse Advice Line (NAL)
plan; developed by collaborative efforts of all designated points-of-contact (POCs) to ensure
program sustainability and reduce variation in standards of practice among various work-
centers. (T-2)
8.1.2. On-going marketing efforts, details of work-centers’ roles and responsibilities,
training, warm handoff processes, information sharing, performance metric reporting, and
process improvement methodologies will be included in the plan.
8.1.3. The plan will be reviewed by the Access Management Team (AMT), forwarded to
Executive Committee of the Medical Staff (ECOMS) for approval and annotated in the
ECOMS meeting minutes. (T-2) The plan will accompany the minutes as an attachment.
8.1.4. Annual review will be conducted to ensure significant changes are incorporated. (T-2)
8.2. NAL Metrics.
8.2.1. NAL updates, booking analysis metric, warm-handoff metric, beneficiaries pre-intent
and NAL recommended disposition metrics, and process improvement efforts will be
reported to the AMT monthly. (T-2) MTFs can report additional metrics if desired.
8.2.2. NAL clinical quality assurance (QA) concerns will be forwarded to Air Force Medical
Operations Agency NAL to determine the need for a formal quality review from NAL
Program Management Office (PMO). QA submissions for Air Force MTFs in enhanced
Multi-Service Markets (eMSM) should be forwarded to the appropriate NAL Leads.
8.2.3. All clinical quality assurance concerns resulting in an unwarranted patient outcome
will be forwarded to AFMOA/SGNE via [email protected] or eMSM NAL Leads
immediately.
8.3. Roles and Responsibilities.
8.3.1. SGN, SGH and SGA will:
8.3.1.1. Collaboratively determine expectations from NAL utilization that will support
MTF’s access to care strategic goals.
8.3.1.2. Collaboratively determine the MTF NAL lead and alternate POCs.
8.3.1.3. The MTF NAL process responsibilities will be shared between clinical and
administrative functions to include the SGN, Family Health Flight Commander, 4A
Functional, GPM, and HCI. An individual in one of these functional areas will be
designated as the lead by the SGN/SGA/SGH.
8.3.1.4. This group will forward all quality assurance submissions, POC updates, clinic
instructions, warm handoff updates, and all other inquires to AFMOA via
[email protected] or eMSM NAL leads.
8.3.1.5. Ensure the selected work-center POCs listed below follows guidance:
AFI44-176 8 SEPTEMBER 2017 25
8.3.2. The Flight Commander or clinical nurse designee from each AFMH clinic will:
8.3.2.1. Provide guidance and oversight for beneficiary follow-up protocols post Urgent
Care Center (UCC) or Emergency Department (ED) visit.
8.3.2.2. Review clinic instructions and warm-handoff contact numbers to ensure
accuracy.
8.3.2.3. Address warm-handoff deficits related to gaps in internal processes.
8.3.2.4. Ensure all personnel designated to respond to warm handoffs are aware of rules
of engagement and daily access capabilities/expectations.
8.3.3. The Appointing Center Supervisor will:
8.3.3.1. Ensure personnel are aware of NAL rules of engagement and daily access
capability/expectations.
8.3.3.2. Address warm-handoff deficits related to gaps in internal processes/workflows
immediately to the MTF NAL POC.
8.3.4. Utilization Managers (UM) will:
8.3.4.1. Track, trend, and analyze the population’s utilization patterns.
8.3.4.1.1. Provide recommendations related to conditions, demographic factors,
outcomes and formulate process improvements accordingly.
8.3.4.1.2. Report trends and metrics to the Executive Committee accordingly.
8.3.5. The Health Care Integrator (HCI) will:
8.3.5.1. Provide population education via appropriate forums such as mandatory briefs,
newcomers briefings, Commanders Calls, community outreach forums and marketing
tools.
8.3.5.2. In absence of an assigned UM, assume the UM’s responsibilities as indicated
above.
8.3.6. TRICARE Operations and Patient Administration (TOPA) will:
8.3.6.1. Assist with population education by facilitating availability of NAL marketing
tools.
8.3.6.2. Forward UCC/ED network provider updates to NAL when discrepancies are
identified.
8.3.7. Education and Training Officer (ETO) or representative will:
8.3.7.1. Provide expertise to enable MTF to meet all training criteria stated in this
guidance.
8.3.8. Information Management (IM) (i.e. Composite Health Care System (CHCS)
administrator and/or Chief Information Officer (CIO)) will:
8.3.8.1. Ensure CHCS accounts are activated or deactivated per guidance of the Defense
Health Agency (DHA) NAL PMO.
26 AFI44-176 8 SEPTEMBER 2017
8.3.8.2. Ensure scheduled and unscheduled CHCS and Application Virtualization
Hosting Environment (AVHE) outages are reported to the NAL.
8.3.8.3. Be prepared to receive account activation and deactivation notifications from the
DHA NAL PMO to facilitate access of NAL staff.
8.4. NAL Sustainment Guidance.
8.4.1. The NAL may be used as a PCM designee to respond to patient urgent care needs 24
hours a day, 7 days a week. Facilities that use the NAL do not need to identify an on-call
provider for this purpose.
8.5. Training.
8.5.1. To ensure continuity within the MTF, NAL should be included in all orientation
checklists for executive leadership and work-centers (i.e. AFMH clinics, appointing centers,
TOPA, Information Management-CHCS administrator, medical management team, etc.)
involved in decision making, workflow and training processes.
8.5.2. Refresher training should be conducted at least once a year to ensure key personnel
are fully aware of all changes to NAL strategic goals, program dynamics, and workflow
processes.
8.6. Guidance on Beneficiary Initiated Contact with MTF.
8.6.1. During normal operations, MTF personnel will not redirect beneficiaries to the NAL
as a substitute for their ability to access their AFMH teams. (T-1)
8.6.2. If the patient states they want to speak to a nurse, the NAL should not be chosen by
MTF staff as the primary option over the beneficiary’s PCM team’s nurse.
8.6.3. If resources are available to provide walk-ins, MTFs will not redirect beneficiaries to
the NAL.
8.6.4. It is appropriate for patients to be transferred to the NAL upon the patient’s request;
however, MTF personnel cannot transfer or tell the beneficiaries to call the NAL if the
individual prefers to seek care with their AFMH team.
8.6.5. Beneficiaries have the option to utilize NAL services 24 hours a day, seven days a
week.
8.7. Guidance on Warm Handoffs.
8.7.1. The MTF will designate phone line(s) and develop workflows (how the MTF routes
calls and provides support staff for maximum effectiveness) to receive NAL warm handoffs.
Per the AFMS NAL Operational Guidance, signed June 2016, a warm handoff is when one
party telephonically connects the beneficiary with another party and both parties verbally
accept the exchange of the beneficiary via the phone line.
8.7.2. The workflow and telephonic resources must support personnel’s capability to answer
the NAL call within 45 seconds.
8.7.3. When the NAL RN triages the patient and if an appointment is needed, the NAL clerk
first attempts to book the patient in CHCS, and if not successful, there is an attempt by the
NAL to make a warm-handoff to the MTF.
AFI44-176 8 SEPTEMBER 2017 27
8.7.4. Personnel assigned to answer the designated warm handoff phone line must be aware
of MTF’s access goals and current access capacity, i.e. providers available, ability to cross
book within the team or across teams; hours of the UCC/ED (if available) and other
applicable access to care protocols during the time of the call.
8.7.5. It is suggested that weekly telephonic technical quality assurance inspections be
performed to ensure full functionality of designated line(s).
8.8. CHCS and Application Virtualization Hosting Environment (AVHE) Guidance.
8.8.1.1. The MTF must provide CHCS account access to NAL nursing staff/clerks. This
provides the NAL appointment booking capability into the MTF’s CHCS platform.
8.8.1.2. The NAL clerks must be given booking access to all AFMH clinics, to include
Family Medicine, Pediatric, Internal Medicine, Flight Medicine, and Personnel
Reliability Program.
8.8.1.3. The MTF staff must ensure NAL profiles are developed to support cross booking
capability, first to the PCM, then to the PCM Team, then to the PCM clinic in order to
recapture the greatest amount of care possible.
8.9. Guidance on Clinic & MTF Closures.
8.9.1. All Clinic and/or MTF closures due to training, weather, etc. must be reported to the
NAL.
8.9.1.1. This enables the NAL to appropriately support and/or route calls from MTF
beneficiaries during closure. Additionally, it helps to reduce skewed data related to the
unsuccessful warm handoff performance metrics. If the NAL is aware of the closure,
they won’t unnecessarily attempt a warm handoff.
8.10. Marketing Guidance.
8.10.1. An effective MTF marketing campaign will enable beneficiaries to establish realistic
expectations of NAL services and enhance comprehension of rules of engagement
contributing to customer satisfaction.
8.10.2. Marketing tools and examples are located on the NAL Kx page.
28 AFI44-176 8 SEPTEMBER 2017
Chapter 9
REFERRAL MANAGEMENT
9.1. General.
9.1.1. All specialty/surgical care and Right of First Refusal (ROFR) referrals/consults will be
managed IAW current AFMS Referral Management Business Rules (BRs), (see attachment
two), and Assistant Secretary of Defense for Health Affairs (ASD (HA)) referral
management (RM) guidance.
9.1.2. The TOPA Flight Commander is responsible for executing the referral management
(RM) process and the Referral Management Center (RMC); GPMs must be familiar with the
referral process. (T-3)
9.1.3. The MTF’s RMC is accountable for managing and tracking referrals generated by the
MTF and ROFR referrals until closure. The referral is considered closed when: the referral is
cancelled/denied; the patient has cancelled/not used the referral; or the referring provider has
received the Clear and Legible Report (CLR). (T-1)
9.1.4. Carepoint Referral Management Suite (RMS) is the only interim electronic RM
application approved by the Military Health System for use by the MTF to transmit and track
all referrals until the MHS GENESIS Electronic Health Record (EHR) is deployed at the
MTF. (T-0)
9.1.5. The MTF Executive staff or designee (not a workgroup) is the approval authority for
the MTF’s Capability and Capacity report (T-1). The MTF’s Capability and ROFR reports
should be as unrestrictive as possible to retain/recapture the maximum number of specialty
care referrals to sustain clinical currency and minimize purchased care costs. These reports
should be updated as needed for accuracy. (T-3) All referral requests will be routed to the
RMC or multiservice market referral center for administrative review, appointing to the
MTF, and processing to the Managed Care Support Contractor (MCSC). Exceptions to this
process shall be approved by the Executive Staff or designee in writing. MTF specialty
clinics exempted by the Executive Staff are responsible for referral review, booking, &
tracking of those referrals. (T-3)
9.1.6. The MTF Executive Staff will provide appointment booking keys to trained, front line
support staff (e.g. in primary care, central appointing, RMC, etc.) in order to support patient-
centered booking into specialty clinics before the patient leaves the MTF. (T-3)
9.1.7. Clinic, RMC and appointing personnel will use the CHCS Appointment Order
Processing function to book initial MTF specialty appointments. (T-1). This CHCS function
links the appointment to the referral and ensures correct tracking through CHCS and RMS.
9.1.8. The MTF Executive Staff will empower appointing agents to book the patient’s
specialty appointment anytime the referral has an “Appoint to MTF” review. If the referral
lacks a review disposition when the patient calls, then the appointment center agent shall
provide the patient a “warm hand-off” to the RMC or specialty clinic to immediately review
the referral and appoint or defer it. If “clinic-book only” appointments are authorized, and a
patient calls the central appointment center for a “clinic book only” appointment, then the
AFI44-176 8 SEPTEMBER 2017 29
appointing agent shall provide a “warm hand-off” directly to the specialty clinic to assist the
patient. (T-0)
9.1.9. The MTF Executive Staff will ensure patients are offered three different specialty
appointment times within the 28 calendar day access to care standard. When the MTF cannot
offer three different specialty appointment times within the access standard, patients may be
offered MTF appointments outside the standard if they choose to waive their ATC standard.
If the patient does not waive their ATC standard, the patient’s referral will be deferred to the
purchased care. (T-0)
9.1.10. The MTF Executive Staff will ensure specialty clinic and RMC personnel return
patient messages within one business day of message receipt. One business day includes the
message received date plus the end of the next business day. (T-0)
9.1.11. The MTF Executive Staff will ensure the MTF’s consult/referral auto-closure
function in CHCS is turned off. (T-0)
9.2. Referring Provider Responsibilities.
9.2.1. The referring provider will:
9.2.2. Promptly enter all initial specialty referrals into the EHR, preferably before the patient
leaves the encounter or immediately after the virtual visit. (T-1)
9.2.3. Review referral results within three business days of notification that the results have
been received. (T-1)
9.2.4. Communicate to the patient within one business day when a referral is denied or
cancelled, and whether or not a new referral will be ordered. This communication may be
delegated to the clinical team. (T-3)
9.3. Specialist Responsibilities.
9.3.1. The specialist will communicate to the referring provider the reasons for a referral
cancellation or if more information is needed on the referral. This communication may be
delegated to the clinical team. (T-3)
9.4. Referral Management Center (RMC) Responsibilities.
9.4.1. The RMC will:
9.4.1.1. Ensure all initial specialty care referrals are either accepted for appointing to the
direct care system or deferred to the network within one business day from the order date.
One business day includes the order date plus the end of the next business day. (T-0)
9.4.1.1.1. For referrals requiring specialty clinic review, if the specialty clinic does
not review the referral within one business day, the RMC will book the patient to the
specialty clinic based on the MTF’s capability/capacity report or defer the patient to
the network. (T-0)
9.4.1.2. Defer TRICARE eligible patient referrals to the network regardless of
beneficiary category or specialty service line if the patient cannot be booked to the MTF
specialty clinic within the appropriate ATC standard as indicated by the referral priority
and the patient does not waive the ATC standard. (T-0)
30 AFI44-176 8 SEPTEMBER 2017
9.4.1.3. Notify patients that their referral was deferred to the network or accepted for
appointing to the MTF within one business day from the time the review decision (e.g.,
Appoint to MTF or Defer to Network) was entered into the EHR. (T-0)
9.4.1.3.1. This communication can occur before the patient leaves the MTF, by live
phone call or secure messaging after the patient leaves the MTF, or through
automated methods (e.g. Audio-Communicator, etc.). The communication will
inform the patient about how to make the direct care appointment, how to cancel the
referral, and/or when to expect the network authorization letter or e-mail. (T-0)
9.4.1.4. Notify the referring provider of all routine priority referrals not used or activated
by their patients IAW local MTF policy, but no less than monthly. (T-1)
AFI44-176 8 SEPTEMBER 2017 31
Chapter 10
AIR RESERVE COMPONENT (ARC) ACCESS TO CARE
10.1. Introduction.
10.1.1. The following DoD and Air Force publications provide guidance for determining
ARC eligibility: AFI 41-210, TRICARE Operations and Patient Administration Functions;
AFI 36-2910, Line of Duty (LOD) Determination, Medical Continuation (MEDCON), and
Incapacitation (INCAP) Pay; AFI 44-170 Preventive Health Assessment; DoDI 1332.18,
Disability Evaluation System (DES), and the Air Force Reserve Command (AFRC) PHA
Guide. In addition, Title 10 USC Section 1074 and Title 37 United States Code, Section 204
as well as AFRC/SG and Air National Guard (ANG)/SG can be used for references.
10.1.2. ARC members who incur or aggravate an injury, illness or disease in the line of duty
while performing active duty, active duty for training or inactive duty for training or while
traveling directly to or from such duty, shall be provided the medical or dental care
appropriate for the condition until the member is found returned to duty, or the injury, illness
or disease cannot be materially improved by further hospitalization or treatment and the
member has been separated as a result of a Disability Evaluation System (DES)
determination. To enter into the DES for a duty-related determination, the member must have
received an In Line of Duty (ILOD) determination for his/her potentially unfitting
condition(s). (T-0)
10.2. ARC Health Care Benefits for Air Force Required Evaluations.
10.2.1. ARC members assigned to ARC Units with sufficient medical assets will receive
their required evaluations (e.g., Periodic Health Assessment (PHA), annual Dental exam,
etc.) from their respective servicing Reserve Medical Unit or Guard Medical Unit or other
approved source. (T-2)
10.2.2. AFRC members attached to Regular Air Force (RegAF) units or assigned to ARC
Units without a servicing AFRC Medical Unit will receive their required AFRC PHA
evaluations from a RegAF MTF or other approved source. (T-2)
10.2.3. Many ARC members travel considerable distances from their home to their unit of
assignment or have limited time to complete these appointments on duty days. When an ARC
member is seen in the MTF, clinic/ancillary services personnel must complete all physical
and ancillary services on the same day as the provider appointment. (T-3) This does not
include the completion of the paperwork, only the actual testing and evaluation.
10.2.4. ARC members residing outside the MTF catchment area or more than 40 miles from
their units’ servicing MTF may also obtain these evaluations from the nearest MTF.
10.2.5. ARC members not on orders normally show as ineligible in DEERS (Defense
Enrollment Eligibility Reporting System); however, this does not preclude the booking of an
appointment for the ARC member by appointing agents. Should further verification of
eligibility be required, appointing agents should contact the ARC member’s unit
administrator/medical representative or consult the MTF access manager.
32 AFI44-176 8 SEPTEMBER 2017
10.2.6. ARC members are not required to be in “military status” to schedule an appointment;
however, they must be in a military status at the time of the examination and must provide
documentation to clinic staff that they are in a military status. Military status is defined as
active or inactive duty status. ARC members with an approved LOD do not need to be in a
military status for examination or treatment. (T-2)
10.2.7. ARC members will have the same level of access for these required evaluations as
RegAF members. (T-0)
10.3. ARC Access to Care for Line of Duty (LOD) Determinations.
10.3.1. Access to care is allowed only for the condition identified for LOD determination,
during the determination of the LOD. In accordance with AFI 36-2910, Line of Duty
Determination, Medical Continuation and Incapacitation Pay, ARC member must provide
documentation of LOD(s) that are in process or have been determined LOD in order to
receive follow-up care (e.g., AF Form 348). (T-3)
10.3.2. Eligibility for continued medical/dental care will be determined by line of duty
findings as specified in AFI 36-2910. According to AFI 41-210, entitlement exists only for
the medical condition determined to be In the Line of Duty (ILOD). An AF Form 348 (-R),
or DD Form 261, Report of Investigation Line of Duty and Misconduct Status, or Interim
LOD with all signature blocks complete, is needed to establish eligibility. The LOD is valid
for care only until the service member is found fit and returned to duty or separated by the
Disability Evaluation System (DES) for the documented medical condition.
10.3.2.1. ARC members will have the same level of access to care as RegAF members
for treatment of those conditions identified in a positive finding for ILOD determination.
(T-0)
10.3.3. ARC members will not be eligible for care when the determination is Not in Line of
Duty (NILOD). (T-0) Care received at this point is at the member’s expense.
10.3.4. According to AFI 36-2910, paragraph 2.3.3., the immediate commander may issue
an Interim LOD determination to establish initial care and treatment pending the final LOD
determination. The Interim LOD determination is comprised of the completed medical
portion of AF Form 348, in accordance with guidance listed in AFI 36-2910, paragraph
2.3.3.3.
10.4. ARC Referrals. ARC members who require follow-up care not in the area where the
initial treatment was rendered are referred to the closest MTF near their home. Appropriate
medical authority from the referring MTF contacts the appropriate medical authority at the
receiving MTF to ensure care is delivered. The referring MTF will notify the member’s
supporting ARC medical unit of the referral action for tracking purposes. (T-1)
10.4.1. Refer ARC members who are serving under Title 10 Contingency, Title 10, or Title
32 orders who are identified with potential duty-related illness or injury in an urgent manner
(72 hour consult), to include maximum utilization of both RegAF and off-base referral sites.
This practice ensures timely identification and access to entitled healthcare prior to the end of
mobilization or contingency orders and without a break in service that can result in loss of
medical benefits.
AFI44-176 8 SEPTEMBER 2017 33
10.4.2. Any care referred outside the MTF is only paid for if the LOD process has been
initiated or completed. In addition, the referral must be coordinated with the Reserve and
Service Member Support Office Great Lakes (R&SMSO-GL) (formerly MMSO) by MTF
staff. (T-1) Coordination with the R&SMSO-GL ensures services are rendered without a
denial of claim.
34 AFI44-176 8 SEPTEMBER 2017
Chapter 11
SPECIALTY CARE
11.1. Overview.
11.1.1. Specialty clinics include but are not limited to: Optometry, Mental Health, Physical
Therapy, Women’s Health, Surgery, Internal Medicine and Pediatric Specialties, etc.
11.2. Schedule Planning and Forecasting.
11.2.1. Unless otherwise noted in this chapter, specialty care clinics will maintain a rolling
180-day calendar (e.g., historical patient utilization patterns, leave, TDY, base exercises,
down days, etc.) to ensure adequate provider and clinic staff availability to meet patient
demand within access standards. (T-0)
11.2.2. The AMT will analyze patient demand utilizing the measures listed in para 2.2.4. (T-
2) Effective management of appointments will maximize patient access to MTF and avoid
purchasing private sector medical care.
11.3. Schedule Implementation and Management.
11.3.1. Clinic leadership will ensure that schedules are released to allow, at a minimum, a
continuous/rolling 180-calendar day supply of available appointments for booking, unless
otherwise noted in this chapter. (T-0)
11.3.2. Clinic leadership will have written processes for appointment schedule change
requests with the goal of minimizing frequent/repeated changes to opened schedules, changes
causing facility cancellations, and rescheduling of patients. (T-3) Appointments will be set up
to auto-reconfigure as applicable, IAW with Chapter 3, Schedule Management, of this AFI.
11.3.3. In coordination with the clinic, unbooked FTR appointments will be converted or
auto reconfigured to SPEC no later than (NLT) 7 days prior to the scheduled appointment
time. (T-1)
11.3.4. Frozen appointments will be released/deleted NLT 72 hours prior to the clinic day.
Appointments will be set up to auto-reconfigure. (T-1)
11.3.5. GPM will provide a daily review of the next clinic day’s appointment availability
and mix to ensure schedules meet patient demand and are adjusted as needed. (T-2)
11.4. Analysis.
11.4.1. Unfilled appointments will be analyzed to determine the root causes: for example,
type of appointment; time appointment offered; in contrast to purchase care leakage for the
same services; detail codes restrictions, etc. (T-2)
11.4.2. Published schedules will be analyzed to determine the effectiveness relative to the
quantity of appointments, over/under supply, seasonality impacts, cancellations, no-shows,
schedule changes, etc. (T-2)
11.4.3. The GPM and RMC will develop a business case analysis to determine effectiveness
of retaining referred care. (T-2)
11.5. Mental Health ATC Management.

AFI44-176 8 SEPTEMBER 2017 35
11.5.1. The GPM will provide at least a monthly consultation on the management of
templates and schedules and the measurement of the Mental Health clinic’s performance in
meeting ATC standards to the leadership and templating/scheduling staff of the Mental
Health clinic. (T-3)
11.5.2. The GPM will ensure overall management of Mental Health access will be IAW AFI
44-172, Mental Health, to include appointment cancellation guidance for Mental Health
patients. (T-0)
11.5.3. MTFs will establish processes to ensure that requests for emergent mental healthcare
are provided on an immediate basis as dictated by the threat. (T-0)
11.5.4. Urgent mental healthcare is provided within 24 hours or less. (T-0) Urgent mental
healthcare includes manifest behavior and/or cut-off scores on the Patient Health
Questionnaire-9 (PHQ-9). Clinics can book these patients into 24HR appointments or walk
them in. Mental Health clinics should utilize CHCS as much as possible for creating
appointments.
11.5.5. Mental Health Clinic Appointment Types. Clinics will use appointment types IAW
the definitions of Chapter 5. Only the following standard appointment types are permitted to
be used: (T-1)
11.5.5.1. Clinics will use 24HR slots to book urgent mental healthcare requests within 24
hours, to include walk-in appointments that need to be seen the same day.
11.5.5.2. Clinics will use SPEC slots to book any initial mental health patients referred
by another provider or clinic, not to exceed 28 days. All new appointments referred by
the BHOP should be SPECS.
11.5.5.3. Clinics will use FTR slots to book follow-up appointments for additional
mental healthcare/course of therapy. Clinics will book these appointments within the
time frame requested by the mental health provider.
11.5.5.4. Clinics will use GRP slots for patients who require group therapies, counseling,
or teaching sessions where a mental health provider will perform the service in a group
setting. The detail code fields can be used to provide further information about the care to
be provided in the group appointment, (e.g., STRESS for a Stress Management Class). A
group appointment should be scheduled per self-referral of the patient, the clinic's or
referring provider's policy or designation.
11.5.5.4.1. Automated Neuropsychological Assessment Metrics (ANAM) GRP
appointment slots can also be used for ANAM assessments for 1 to 50 personnel
being scheduled during the same time slot. To clarify the care being provided in this
group appointment, it is recommended that two additional detail codes be used in
combination with the GRP standard appointment type. This alerts appointing agents
to book the proper individuals into these slots. This coding also provides a
mechanism to monitor the number of ANAM assessments being performed. They
are:
11.5.5.4.1.1. For Pre-deployment Assessments: Use MH detail code (for Mental
Health) combined with the RPRE detail code (for Readiness Pre-Deployment).
11.5.5.4.1.2. For Post-deployment Assessments: Use the MH detail combined

36 AFI44-176 8 SEPTEMBER 2017
with the RPD (Readiness Post-deployment) detail code.
11.5.5.5. Clinics will use ROUTINE slots to book new self-referrals and not just for
those patients discharged from an inpatient facility.
11.5.6. Behavioral Health Optimization Program (BHOP) Appointing. Military Treatment
Facilities should attempt to utilize BHOP services as entry point for Mental Health services.
11.5.6.1. Appointment types for BHOP: Family Health Clinic embedded service BHOP
clinics are permitted to use three standard appointment types:
11.5.6.1.1. Clinics will use 24HR slots to book urgent behavioral healthcare requests
within 24 hours, to include walk-in appointments that need to be seen the same day.
(T-1)
11.5.6.1.2. Clinics will use the FTR appointment type for patients requesting non-
urgent follow up services, beyond 24 hours only. Follow-up appointments will be
booked within the time frame requested by the BHOP provider. (T-1)
11.5.6.1.3. Clinics will use the GRP appointment type for patients who require
therapy, counseling, or teaching sessions where a provider performs the service in a
group setting. (T-1)
11.5.6.1.4. Clinics will use the SPEC appointment type for all new appointments. (T-
1)
11.5.6.2. WALK-IN visits are also allowed and clinics will use when a patient urgently
needs to be seen and there is no appointment available. (T-1)
11.5.7. Mental Health should have a no-show rate of no more than five (5) percent for new
SPEC appointments and no more than ten percent for all other appointment types. (T-1)
11.6. Physical Therapy (PT) Direct Access Management.
11.6.1. Appointment Types Used in PT Templates and Schedules. Appointment types will
be used as outlined below: (T-3)
11.6.1.1. Clinics will only use 24HR slots to schedule direct access (i.e., no referral
needed) evaluations and for acute conditions that should be seen within 24 hours.
11.6.1.2. Clinics will use SPEC slots to schedule/book any Routine priority
referral/consult requests for initial physical therapy care evaluations by a physical
therapist (officer or civilian/contract equivalent) within the time frame requested by the
referring provider or not to exceed 28 days. (T-3)
11.6.1.3. Clinics will use FTR slots to schedule/book appointments to the physical
therapist for the purpose of reevaluation or treatment. Clinics will book these
appointments within the time frame requested by the physical therapist. (T-3)
11.6.1.4. Clinics will use PROC slots to schedule PT care appointments to enlisted,
civilian, or contract PT technicians or equivalent providers as approved/directed by the
physical therapist. The majority of appointments scheduled for PT technicians will use
the PROC appointment type. If multiple patients are to be seen at the same time by the
PT Technician in a group setting for PT care/courses of therapy, the PROC appointment
AFI44-176 8 SEPTEMBER 2017 37
type with multiple appointment slots during the same time will be used. Clinics will book
all PROC appointments within 28 days to meet the Specialty Care ATC standard. (T-3)
11.6.1.5. Clinics will use GRP slots for patients who require group teaching/education
classes/sessions by any physical therapist or PT technician. (T-3)
11.6.2. Guidance if Physical Therapist and PT Technician treat patient during same visit:
11.6.2.1. If both the physical therapist and the PT technician see a patient during a visit,
the appointment type used will default to the one that was originally chosen when
booking the appointment. For example, if a PROC appointment is booked for the PT
tech, but during the visit the physical therapist sees the patient, then the appointment type
for the visit remains PROC.
11.6.3. Physical Therapy should have a no-show rate of no more than five (5) percent for
new SPEC appointments and no more than ten percent for all other appointment types. (T-3)
11.7. Audiology/Hearing Conservation ATC Management.
11.7.1. Audiology/Hearing Conservation scheduling must adhere to all of the operational
definitions. (T-3)
11.7.2. Clinics will schedule Hearing Conservation (Audiology) encounters in the FBNA
MEPRS clinic regardless of appointment type booked. (T-3)
11.7.3. Clinics will schedule Clinical Audiology encounters in the BHDA (Primary Medical
Care - Audiology) MEPRS clinic regardless of appointment type booked. (T-3)
38 AFI44-176 8 SEPTEMBER 2017
Chapter 12
ACCESS TEAM TRAINING, MANAGEMENT AND TRAINING RESOURCES
12.1. Management and Training of GPMs:
12.1.1. To ensure that the GPM is optimally trained for the position, GPMs must attend the
resident AFMS GPM Orientation Course conducted at the Medical Education and Training
Campus (METC) within two to four months of assuming the GPM position. (T-2)
12.1.2. The GPM will attend an Access Improvement Seminar during the first year of each
assignment as a GPM. (T-2)
12.1.3. GPMs will attend the Air Force Medical Home Operations (AFMHO) Course within
6 months of assignment as a GPM. (T-2)
12.1.4. GPMs will attend the Appointing Information Systems Hands-on Training Course
during their first assignment as a GPM. (T-2)
12.1.5. GPMs will remain in the position no less than 2 years. (T-3)
12.1.6. GPMs will attend the annual GPM symposium or as scheduled. (T-3)
12.2. Training of Appointing Agents:
12.2.1. MTFs will establish and require initial and annual refresher appointing training for
all personnel who have CHCS booking keys. (T-3)
12.2.2. Evidence of required training will be documented and tracked within the MTF. (T-3)
AFI44-176 8 SEPTEMBER 2017 39
Chapter 13
TRICARE ONLINE
13.1. TRICARE Online (TOL) Overview.
13.1.1. TRICARE Online is an enterprise-wide, secure, internet portal for use by all DoD
beneficiaries, providers, managers, managed care support contractors, and worldwide
medical support staff to access available healthcare services, benefits, and information. TOL
is a scalable, open standards platform upon which other applications can be integrated.
13.1.2. MTF leadership and commitment are vital to the success of TOL adoption,
implementation and sustainment. MTF Commanders should appoint experienced,
empowered, and motivated personnel to serve in key TOL team leadership positions.
13.2. TRICARE Online Roles and Responsibilities.
13.2.1. Air Force TOL Functional Program Manager. The Air Force TOL functional
program manager is located at AFMSA/SG3S and provides program policy direction and
functional requirements expertise to the AFMSA/AFMOA Information Management offices
to help them manage and sustain the technical aspects of the TOL system. Responsibilities
include:
13.2.1.1. Provide support to Defense Health Agency (DHA) TOL Program Management
as the AFMS Functional Service Program Manager/ Stakeholder.
13.2.1.2. Support/coordinate technical maintenance efforts with AFMS Information
Management Office in accordance with service guidelines.
13.2.1.3. Coordinate processes needed to receive, develop and approve systems change
requests and new requirements received from AFMSA, AFMOA, MAJCOM and/or MTF
level functional personnel.
13.2.1.4. Submit/coordinate new TOL system change requests/requirements on behalf of
the AFMS to DHA and coordinate on new requirements submitted by the other Services.
13.2.1.5. Coordinate the final development of necessary metrics/measures of appointing
operations performance with applicable AF and DHA organizations.
13.2.1.6. Maintain an MTF TOL Appointing Subject Matter Expert (SME) list that is
updated at least semi-annually.
13.2.1.7. Coordinate with the DHA Program Office to grant TOL System Administrator
rights to those designated/listed as an SME.
13.2.1.8. Attend TOL related meetings (e.g., Program Management meeting, sustainment
meeting, and various joint-service configuration management working groups).
13.2.1.9. Provide guidance to Air Force Inspection Agency (AFIA), AFMOA,
MAJCOM Command Surgeons, and/or MTFs in the area of TOL functions.
13.2.1.10. Review marketing, training, and support materials for release to AFMS
organizations and MTFs.
13.2.1.11. Coordinate training with AFMSA and/or MTFs.
40 AFI44-176 8 SEPTEMBER 2017
13.2.1.12. Coordinate upgrades of new TOL capabilities with DHA TOL Program
Office, AFMOA, MAJCOMs and MTFs.
13.2.1.13. Coordinate applicable system security, information assurance certifications
with DHA, AFMSA and/or necessary AFMOA offices as needed to ensure that
applicable documents such as Authority to Connect, Authority to Operate and other
system security certifications are approved to support secure TOL system operations.
13.2.2. AFMSA Access to Care Program. AFMSA Access to Care Program has the role of
maintaining the policy pertaining to the TOL roles and responsibilities for the AFMS.
13.2.3. AFMOA Health Benefits Division (AFMOA/SGAT). The AFMOA Office
coordinates with the AFMSA/SG3S TOL functional program management office regarding
program and system implementation and sustainment requirements. Responsibilities of this
office include:
13.2.3.1. Serves as AFMSA TOL program implementation and sustainment point of
contact (POC).
13.2.3.2. Maintains an MTF identified TOL System Administrator listing that is updated
at least semi-annually.
13.2.3.3. Forwards the updated/completed listing to AFMSA/SG3S, Operations Element,
who will coordinate with the DHA Program Office to grant TOL System Administration
(SA) rights.
13.2.4. MTF Responsibilities. The MTF leadership appoints and empowers personnel to fill
the TOL sustainment team positions, to include a TOL Program Manager, MTF TOL System
Administrator (SA), MTF TOL Appointing Subject Matter Expert (SME) and TOL
Marketing POC. (T-3)
13.2.4.1. MTF TOL Program Manager. Personnel fulfilling this role are assigned to the
TOPA function at the MTF. Responsibilities include:
13.2.4.1.1. Coordinate TOL account permissions and facilitate account
activation/changes for TOL users. (T-3) Partner with pharmacy to ensure that TOL
pharmacy features are reviewed regularly and are enabled for patient use.
13.2.4.1.2. Establish business practices to incorporate TOL registration into venues
such as the newcomer orientation or Right Start process for newly assigned base
personnel. (T-3)
13.2.4.1.3. Attend Medical Group (MDG) staff meetings as appropriate to
disseminate new TOL information. Examples include TOL system updates, system
downtimes, new tools, etc. (T-3)
13.2.4.1.4. Complete all applicable training pertaining to the TOL System,
functionality, and user accounts. Initial and annual training will be provided by
AFMSA/SG3S. (T-1)
13.2.4.1.5. Ensure appointment letter/MDG POC listings are updated for MDG staff
to be aware of the individual(s) fulfilling the MTF TOL SA role. (T-3)
AFI44-176 8 SEPTEMBER 2017 41
13.2.4.1.6. Work with MTF TOL Marketing POC to ensure successful marketing to
the base populace. (T-3)
13.2.4.2. MTF TOL System Administrator. Personnel fulfilling this role are assigned to
the Information Systems Flight at the MTF. Responsibilities include:
13.2.4.2.1. Review/understand the MTF Server Installation and Configuration Guide
and basic TOL features that can be obtained from the Science Applications
International Corporation (SAIC®) personnel at the MTF to ensure the proper
operations of the TOL system. (T-3)
13.2.4.2.2. Coordinate with the MTF TOL Program Manager and the AFMOA
Health Benefits Division to assist/provide oversight with TOL hardware and software
installation activities. (T-1)
13.2.4.2.3. Resolve TOL system/technical issues at the MTF level as needed. (T-3)
13.2.4.2.4. Serve as coordinator when changes/maintenance to CHCS, or any other
network, impacts the overall operation of TOL. (T-3)
13.2.4.2.5. Coordinate with the MTF TOL Program Manager to ensure MTF is ready
for new capability interfaces. (T-3)
13.2.4.2.6. Ensure the maintenance of the MTF TOL system to include all aspects
except appointing functions.
13.2.4.3. MTF TOL Appointing SME. Personnel fulfilling this role are assigned to the
GPM office. Responsibilities for this role include:
13.2.4.3.1. Understand how to prepare, monitor, and maintain CHCS appointing
schedules to maximize TOL’s web-enabled appointing functionality. (T-3)
13.2.4.3.2. Work with MTF appointing staff, the MTF TOL Program Manager and
SA and the AFMSA/SG3S TOL Functional Program Office, to maximize the MTF’s
TOL appointing functions. (T-1)
13.2.4.3.3. Serve as the MTF POC when changes to the CHCS appointing templates
impact TOL, appointing functionality, or when new appointment functionality is
added to TOL. (T-3)
13.2.4.3.4. Ensure the MTF clinic personnel understand the TOL appointing business
rules. (T-3)
13.2.4.3.5. Ensure that at least 80 percent of all CHCS appointment slots in primary
care clinics, to include Family Health , Pediatrics, Internal Medicine, Flight Medicine
and Optometry clinics schedules, are available/viewable for booking in TOL
appointment schedules IAW Chapter 3 and Chapter 5 of this AFI. (T-1)
13.2.4.3.6. Management of TOL Scheduling and Appointment Management will be
governed IAW Chapter 3 and Chapter 5 of this AFI. (T-1)
13.2.4.4. TOL Marketing POC. The Marketing POC performs one of the most critical
functions for TOL sustainment. MTF staff and beneficiary knowledge about TOL is
crucial to the success of the program and/or any new application releases on TOL.
Responsibilities of this role include:
42 AFI44-176 8 SEPTEMBER 2017
13.2.4.4.1. Develop and organize a marketing strategy that targets the MTF‘s various
patient groups. (T-3) This strategy includes: having providers and clinic staff act as
informal promoters of TOL, utilizing available resources (e.g., newsletters, on-hold
telephone messages, installation newspapers) to market TOL, coordinating with MTF
TOL Appointing SME to develop marketing strategies specific to clinic (e.g.,
pediatric vs. adult medicine clinic), and/or supplying marketing materials to clinics
throughout the MTF, and across the base. (T-3) The MTF TOL usage goal is no less
than 5%.
13.2.4.4.2. Redefine marketing strategies for specific clinics as needed as well as
when new TOL capabilities and changes develop. (T-3)
13.2.4.4.3. Attend marketing meetings with the TOL Program Office, MAJCOM
and/or AFMOA TOL POC, and AFMSA/SG3S. (T-1)
MARK A. EDIGER, Lieutenant General, USAF,
MC
Surgeon General
AFI44-176 8 SEPTEMBER 2017 43
Attachment 1
GLOSSARY OF REFERENCES AND SUPPORTING INFORMATION
References
10 USC Sections 1074, 1078
Title 32 Code of Federal Regulations, 199.17
37 USC §204
DoDI 1241.2, Reserve Component Incapacitation System Management, 30 May 2001 DoDI
1332.38 Physical Disability Evaluation, 10 April 2013
DoD 6025.18-R, DoD Health Information Privacy Regulation, 24 January 2003 DoD 8580.02-R,
DoD Health Information Security Regulation, 12 July 2007
ASD (HA) 11-005, TRICARE Policy for Access to Care and Prime Service Area Standards, 23
February 2011
AFI 33-360, Publications and Forms Management Guidance Memorandum, 30 November 2016
AFI 36-2910, Line of Duty (LOD) Determination, Medical Continuation (MEDCON), and
Incapacitation (INCAP) Pay, 08 October 2015
AFI 41-210, TRICARE Operations and Patient Administration Functions, 06 June 2012
AFI 44-102, Medical Care Management and Guidance Memorandum, 06 January 2017
AFI 44-119, Medical Quality Operations, 16 August 2011
AFI 44-170, Preventive Health Assessment, 30 January 2014
AFI 44-171, Patient Centered Medical Home Operations, 28 November 2014
AFI 44-172, Mental Health, 13 November 2015
AFI 46-101, Nursing Services and Operations, 30 January 2015
AFI 48-101, Aerospace Medicine Enterprise, 08 December 2014
AFI 48-123, Medical Examinations and Standards and Guidance Memorandum, 19 September
2016
AFMAN 33-363, Management of Records, 21 July 2016
AFPD 44-1, Medical Operations, 9 June 2016
College of American Pathologists, Laboratory Accreditation Program, Standards for
Accreditation, 2015 Edition, December 2015
2016 Accreditation Handbook of the Accreditation Association of Ambulatory Health Care 2016
Practice Guidelines and Technical Standards, American College of Radiology
The Joint Commission National Patient Safety Goals (NPSG) (CAMAC / Ambulatory Health
Care) Goal 1 - 01.01.01, 1 January 2017
44 AFI44-176 8 SEPTEMBER 2017
Prescribed Forms
None
Adopted Forms
AF Form 847, Recommendation for a Change of Publication
Abbreviations and Acronyms
AAAHC—Accreditation Association for Ambulatory Health Care
ACD—Automated Call Distribution
ADSM—Active Duty Service Member
AF—Air Force
AFI—Air Force Instruction
AFMSA—Air Force Medical Support Agency
AFMH—Air Force Medical Home
AFMS—Air Force Medical Service
AFRC—Air Force Reserve Command
AHLTA—Armed Forces Health Longitudinal Technological Application
AMDS—Aerospace Medical Squadron
ANG—Air National Guard
ARC—Air Reserve Component ATC—Access to Care
AVHE—Application Virtualization Hosting Environment
BHOP—Behavioral Health Optimization Program
BR—Business Rules
CHCS—Composite Health Care System
CSSP—Clinical Support Staff Protocol
DART—Direct Access Reporting Tool
DEERS—Defense Enrollment Eligibility Reporting Systems
DoDD—Department of Defense Directive
DoDI—Department of Defense Instruction
EOD—End-Of-Day Processing
GPM—Group Practice Manager
HA—Health Affairs
HCI—Health Care Integrator
IMA—Individual Mobilization Augmentee
AFI44-176 8 SEPTEMBER 2017 45
Kx—Knowledge Exchange
LOD—Line of Duty
LWOBS—Left Without Being Seen
MCSC—Managed Care Support Contractor
MDOS—Medical Operations Squadron
MDSS—Medical Support Squadron
MEPRS—Medical Expense Reporting and Performance System
MHS—Military Health System
MTF—Military Treatment Facility
NAL—Nurse Advice Line
OSD—Office of the Secretary of Defense
PCM—Primary Care Manager
PHA—Preventive Health Assessment
PT—Physical Therapy
RC—Reserve Component
RMC—Referral Management Center
RM—Referral Management
RMS—Referral Management Suite
ROFR—Right of First Refusal
SGA—Administrator
SGH—Chief, Medical Staff
SGN—Chief Nurse
TJC—The Joint Commission
TM—Template Manager
TOL—TRICARE On-Line
TOC—TRICARE Operations Center
TOM—TRICARE Operations Manual
TOPA—TRICARE Operations and Patient Administration
TRC—TRICARE Regional Contractor
46 AFI44-176 8 SEPTEMBER 2017
Attachment 2
AFMS REFERRAL MANAGEMENT (RM) BUSINESS RULES (BRS)
Table A2.1. Numbered Decision Points.
No.
Decision Point
Description
Tier
1.
RMC Staff
Training
At a minimum, the Referral Management Center (RMC) staff
will:
Read and refer to AFI 44-176, RM guidance/policies, other
AFIs impacting referrals; TRICARE Operations Manual
(TOM) chapters related to referrals; TRICARE Policy
Manual (TPM) on the TRICARE benefit.
Complete Referral Management Suite (RMS) and Electronic
Health Record (EHR) training (CHCS or MHS GENESIS);
Managed Care Support Contractor (MCSC) website/tools
training; other MTF training.
T-2
2.
Locate RMC
w/Patient In
Mind
The RMC should be located within the MTF (exception:
Enhanced Multi-Service Markets (eMSM)) and in close
proximity to the primary care clinics to promote patient
convenience and staff communication. The RMC location
will be configured to accommodate queues and patient
privacy.
3.
Educate MTF
Providers &
Clinical Staff
The MTF will train providers/clinical staff during
orientation/in-processing and on a recurring basis as needed
on the following: roles and responsibilities for ordering
referrals/consult; specialty capability within the MTF/
eMSM; non-covered benefits to avoid writing referrals that
will be denied; use of network specialists; and avoidance of
MTF directed referrals and use of non-network specialists
without written clinical justification.
T-3
4.
Consult and
Referral
Definitions and
Priority Types
Definition of a consult: a request for an opinion on the best
course of treatment for a patient; the referring provider
continues care for patient based on the advice of the
consulted provider. Example: Evaluate Only
Definition of a referral: a request to evaluate and treat and
assume care for the patient for the condition. The terms
referrals and consults are used interchangeably in this
document. Example: Evaluate and Treat
T-3
4.1.
Other than
Routine Priority
Specialty Care
Referrals
For other than routine priority referrals, the provider/clinical
team will contact the specialist directly and arrange an
appointment (hand-off communications). The accepting
provider’s name, appointment date, phone number (if
T-1
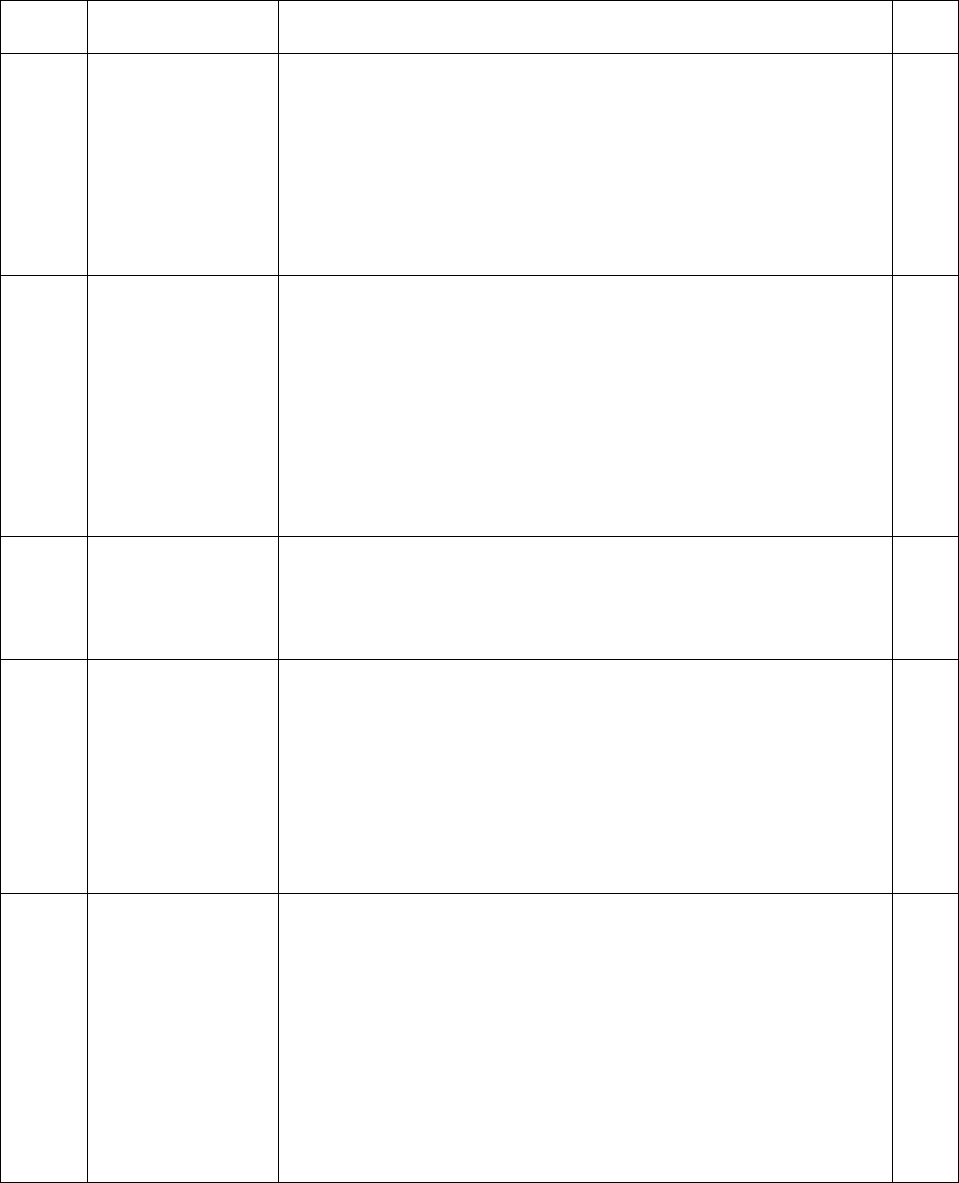
AFI44-176 8 SEPTEMBER 2017 47
No.
Decision Point
Description
Tier
available) and location/facility will be annotated within the
referral. Urgent Care is defined in the TOM as “medically
necessary treatment that is required for illness or injury that
would not result in further disability or death if not treated
immediately. The illness or injury does require professional
attention, and should be treated within 24 hours to avoid
development of a situation in which further complications
could result if treatment is not received.”
4.2.
For urgent priority referrals, the provider/clinical team will
contact the specialist directly and arrange for an urgent
specialty care appointment (hand-off communication).
Alternatively, the MTF’s MCSC can assign a specialist. The
RMC will process the referral immediately and transmit it to
the MCSC. The RMC/clinical team will ensure the patient
clearly understands when and where his/her urgent priority
referral appointment will occur per the MCSC authorization,
before leaving the MTF.
T-1
4.3.
Routine Priority
Referrals
The DoD access to care (ATC) standard for routine referrals
is 28 days from date the referral was written. See BR 10,
“Appoint Referral to MTF Specialty Clinic”, for waiving
ATC standards.
4.4.
Urgent Primary
Care Referrals
The MTF will manage and track consults for urgent primary
care. Urgent primary care consults requested during or after
duty hours will be entered into the EHR NLT the next duty
day. With documented training and written algorithms, other
staff members (e.g., appointing agents, etc.) may enter
consults for urgent primary care into the EHR. The RMC
will transmit the consult to the MCSC and obtain the urgent
primary care consult results.
T-1
4.5.
Urgent Primary
Care Pilot
For the allowed number of urgent primary care visits without
a referral for eligible beneficiary categories per TRICARE
policy, refer to TOM, Chapter 18, Section 19, Pilot Program
On Urgent Care For TRICARE Prime/TPR Beneficiaries.
Urgent care (UC) sought under this program is considered a
“self-referral” episode of care; there is no requirement to
chase the UC report. However, MTFs should encourage
Urgent Care Clinics (UCCs) to send results to the MTF. UCC
Reports to be obtained by the MTF though means such as the
NAL.
48 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
5.
Order Referral
Credentialed providers will order consults in the EHR before
the end of the patient encounter so the patient can go to the
RMC for appointing, guidance/counseling before he/she
leaves the MTF. At a minimum, providers should include on
the referral: a provisional diagnosis; reason for referral to
include treatments attempted and outcome(s); care or service
requested; and whether the specialist is to evaluate or
evaluate and treat the patient.
T-1
5.1.
Referral
Renewals,
Retroactive
Referrals
The RMC staff will not enter new, renewal, or retroactive
referrals/consults (excludes ROFRs). For requests by network
specialists for additional visits, per TOM Chapter 8, Section
5, “For services beyond the initial authorization, the MCSC
shall use its best practices in determining the extent of
additional service to authorize. The MCSC shall not request a
referral from the MTF…” This applies for non-ADSM
patients. ADSM patients require MTF approval and referral
renewal.
T-1
5.2.
Provider By
Name, Directed,
and Non-
Network
Referrals
The MTF will not direct referrals to specific network or non-
network providers (Provider by Name) without written
clinical justification. The MTF will not direct referrals to
providers greater than 100 miles from the MTF (Directed
Referrals) and coordination with the TRO (See TOM,
Chapter 8, Section 5). Patients requesting specific non-
network providers may exercise their point of service option
or contact the MCSC.
T-0
5.3.
Non-Covered
Benefits
If a referral is ordered for a non-covered benefit, the MTF
will submit to the MCSC the Defense Health Agency (DHA)
waiver approval with the referral. If the waiver approval is
not included when the referral is sent, the MCSC will deny
the referral. Resources: The MCSC will use the No
Government Pay List (NGPL) and TRICARE Policy for
included/excluded services to administer the TRICARE
benefit for ADSMs (See TOM, Chapter 17, Section 3,
Contractor Responsibilities, for complete policy
http://manuals.tricare.osd.mil/). The NGPL is available on
the www.health.mil site.
T-0
5.4.
Waiver for Non-
Covered Benefit
Waiver forms, DHA policy, and AF waiver process can be
downloaded from the AFMS Knowledge Exchange. Contact
the AFMOA/SGAT region POC for questions. In general, the
requesting provider and the MTF SGH will initiate the
waiver process and complete required documents. Forward
waiver to the AF Consultant that provides guidance for the
AFI44-176 8 SEPTEMBER 2017 49
No.
Decision Point
Description
Tier
specialty requested. If the AF Consultant does not support
the waiver, do not forward to AFMOA SGAT. If the AF
Consultant approves the waiver, forward package to the
respective AFMOA SGAT Regional Rep. Once the waiver is
approved by DHA, the RMC will fax the approved waiver
with the referral to the MCSC.
6.
Route Referrals
to RMC
The MTF will route all specialty care referrals through the
EHR to the RMC or eMSM RMC for administrative review,
appointing to the MTF, and processing. The Executive Staff
will approve in writing exceptions to this routing. MTF
specialty clinics (exempted by the Executive Staff) that
perform their own reviews will be responsible for referral
review, booking, and tracking of referrals.
T-1
6.1.
RMC CHCS
“Clinic”
MTFs will configure the RMC as a “Clinic” location Hospital
Location file, use ELAA MEPRS code and populate the
“Clinic Specialty” field with all clinic specialties available in
the MTF and purchased care.
T-1
6.2.
CHCS Ancillary
Procedures
The MTF will ensure that each Ancillary Procedure contains
the name of the specialty in the “Clinic Specialty” field and
the RMC in the “Consulting Clinic” field. Applies only for
specialty care referrals as defined in BR 4.
T-1
6.3.
Orders Entered
as “Referrals”
For orders or requests for care that use the EHR as means to
track orders performed in the purchased care and do not
require a MCSC authorization (e.g, mammograms for Non-
ADSMs, case management, laboratory requests, etc.), the
MTF will route the “referral” to the appropriate MTF
accountable tracking owner. See BR 13.5
T-1
7.
Send Patients to
the RMC
Referring providers/clinical teams will instruct patients with
referrals to go to the RMC prior to leaving the MTF
(Exception: eMSM RMCs located at a distance from the
referring MTF). The MTF should provide patients a brochure
which explains, at a minimum, the RM process, contact
information of MCSC for authorization questions, and
RMC’s contact information for questions.
T-3
8.
Customer
Service
RMC staff will confirm patient’s TRICARE eligibility and
contact information (in CHCS, ensure preferred phone
number is entered in the “home phone number” field);
appoint the patient’s MTF specialty appointment prior to
leaving the MTF or explain how they will be notified of their
appointment; and explain the purchased care referral process.
Refer the patient to the MCSC or Beneficiary Counseling and
T-3
50 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
Assistance Coordinator for health plan coverage information
as needed.
9.
Referral Review
The RMC will review all specialty care referrals (except self-
referrals and “referrals” for administrative tracking) within
one business day from the date the referral was ordered. One
business day includes the order date plus the entire following
day, excluding weekends and holidays. The review process
includes checking the MTF’s capability/capacity report and
appointing guidelines to determine if the referral can be
appointed to the MTF. The RMC staff should consult with
subspecialty clinics or send the referral to the specialist for
review as needed. If the MTF has no capability/capacity for
the requested specialty, the RMC will defer the referral to
the purchased care. The RMC will ensure the referral
includes the required data elements as defined in TOM
Chapter 8 Section 5.
T-0
9.1.
Specialty Clinic
Review
If the referral requires a review by the specialty clinic, the
specialty clinic will review the referral within one business
day from the date the referral was ordered. One business day
includes the order date plus the entire following day,
excluding weekends and holidays. If the specialty clinic does
not review the referral within one BD, the RMC will book
the patient to the specialty clinic based on the MTF’s
capability/capacity report and appointing guidelines or defer
the patient to the network.
T-1
9.2.
Incomplete
referrals
The RMC may complete missing information or over-ride
incorrect fields in RMS or MHS GENESIS, if permitted;
otherwise, the RMC should return the referral to the ordering
provider for correction and/or completion.
10.
Appoint
Referral to
MTF
To the greatest extent possible, the MTF will book patients to
the MTF’s specialty care clinic before the patient leaves the
MTF.
T-0
10.1.
Specialty Clinic
Appointing
Guidelines
Specialty clinics will provide the RMC and eMSM RMC
with current appointing guidelines. The appointing
guidelines should be as unrestrictive as possible to
retain/recapture the maximum number of specialty care
referrals within the MTF.
T-3
AFI44-176 8 SEPTEMBER 2017 51
No.
Decision Point
Description
Tier
10.2.
Access To Care
(ATC)
The MTF will book the initial specialty appointment IAW
DoD ATC standards (32 CFR Section 199.17). If the MTF
cannot meet the ATC standard, the appointing staff should
ask patients if they would like to waive their ATC standard
and opt for a later appointment. MTFs cannot mandate
patients to waive their ATC standard. If the patient does not
waive his/her ATC standard, then the MTF will defer the
patient to purchased care.
T-0
10.3.
Appointing in
the EHR
The MTF will book the initial MTF specialty appointment in
CHCS using the Appointment Order Processing (AOP)
function in order to link the appointment with the referral and
ensure correct tracking through CHCS/RMS. Follow MHS
GENESIS procedures to appoint patients.
T-0
10.4.
Contact Patients
The MTF will notify patients of their MTF referral
appointment before they leave the MTF or within one
business day from the date the review decision to appoint the
referral to the MTF was made. The notification can be done
by live phone call, secure messaging, or through automated
methods (e.g. Audio-Communicator, etc.). The notification
will be repeated until the appointment is booked, the patient
cancels the referral, or the message has been delivered three
times on separate days.
T-0
11.
Referrals to
Another MTF
(CHCS)
MTFs that refer patients to other MTFs should follow the
following processes:
a. If the referring MTF (e.g., Bolling AFB) is on the
same CHCS host as the consulting MTF (e.g.,
Andrews AFB), the referring MTF (Bolling) should
select the consulting clinic (e.g., Andrews RMC) and
enter a review status of “Refer to Subspecialty” (code
14).
b. If the referring MTF (e.g., Laughlin AFB) is not on the
same CHCS host as the consulting MTF (e.g.,
SAMMC Consult & Appointing Office (CAMO)),
the referring MTF (Laughlin) should enter a review
status of “Defer to Network” (code #10) and in the
first line of the “Review Comment” field will type
“To MTF/” plus the DMIS of the consulting MTF,
e.g. TO MTF/0066. Complete the Clinic specialty
field, indicating the specialty requested. Transmit the
referral to the consulting MTF. The consulting MTF’s
RMC (e.g., CAMO) should enter the referral in
CHCS/AHLTA as a consult and in the first line of the
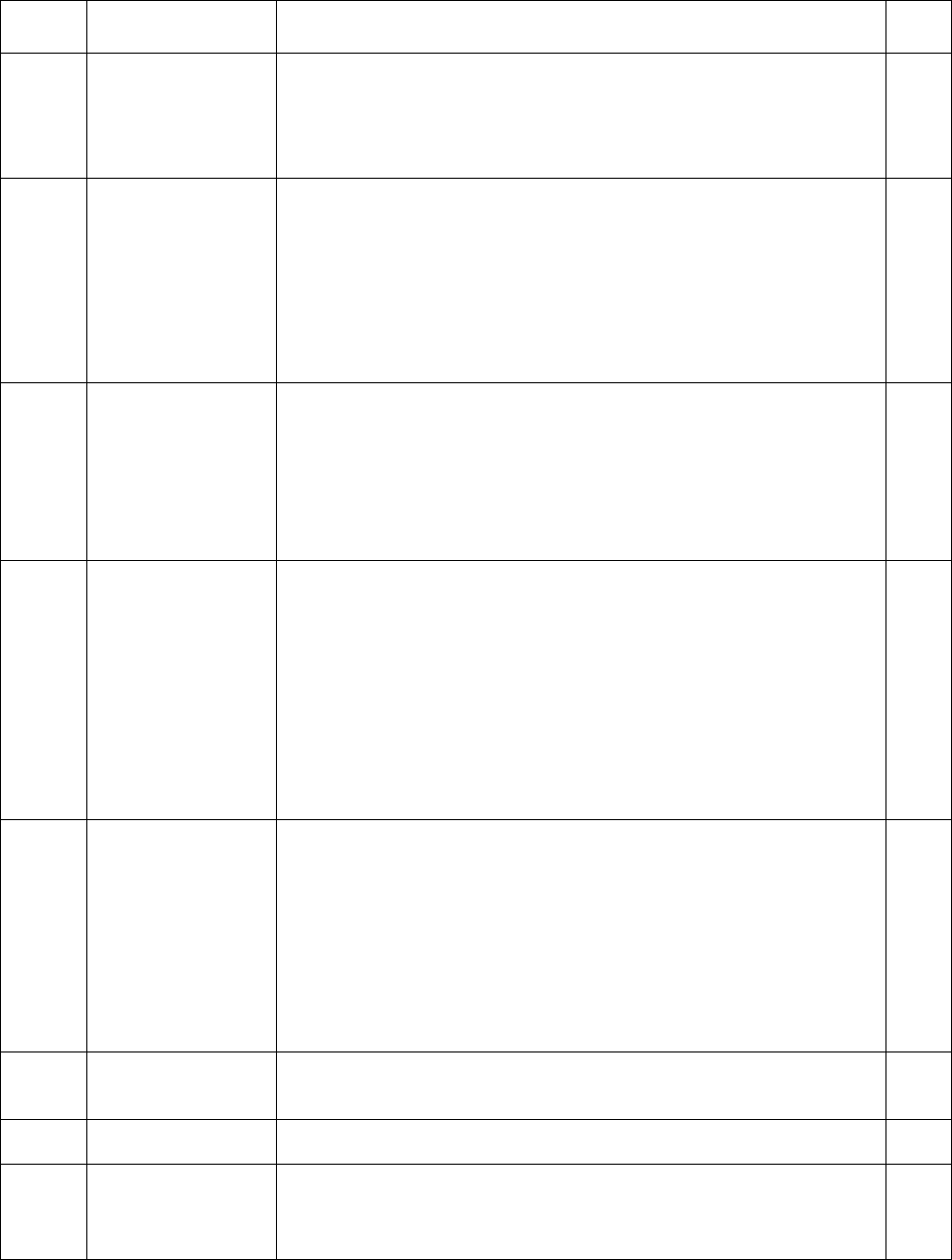
52 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
Review Comment field will type “From MTF/” plus
the DMIS of the referring MTF, e.g., FROM
MTF/0114. Follow MHS GENESIS procedures.
12.
MTF
Capability and
Capacity Report
The MTF Executive Staff will approve the MTF’s Capability
and Capacity report. The MTF’s Capability and Capacity
report should be as unrestrictive as possible to
retain/recapture the maximum number of specialty care
referrals to sustain clinical currency and minimize purchased
care costs. The MTF will ensure the report is current and
provided to the RMC, MCSC, and eMSM (if applicable).
T-1
13.
Defer Referral
to Purchased
Care
When there is no specialty care available in the MTF, the
RMC or eMSM will defer and transmit the referral to the
MCSC. The RMC will assist patients with specialty care
referrals not requiring MCSC authorization and advise them
of their options based on their TRICARE health plan and
eligibility.
T-0
13.2.
Patient Contact
The MTF will notify patients of their defer to network
referral before they leave the MTF or within one business
day from the date the review decision to send the referral to
the purchased care was made. The notification can be done
by live phone call, secure messaging, or through automated
methods (e.g. Audio-Communicator, etc.). Repeat the call 14
calendar days after the referral’s order date to remind the
patient to make an appointment with the civilian provider
indicated in the authorization letter.
T-0
13.3.
Document
Reasons for
Deferring a
Referral to the
Purchased Care
The RMC will document at least one of the below codes in
the referral’s CHCS Review Comment field using the hard
brackets [xx]. Use of at least one code is mandatory. Multiple
codes may be used; however, each code must be in its own
bracket. MTFs should utilize the RMS “Referral Summary”
or “Referral Trends” reports to analyze reasons referrals were
sent to the purchased care. MTFs on MHS GENESIS will
follow MHS GENESIS processes.
T-1
13.3.1.
[2nd]
Second opinion requested. Patient or provider requested a
second opinion
13.3.2.
[CB]
Capability. MTF did not have specialty or services requested
13.3.3.
[CC]
Continuity of Care: Continuity of care is operationally
defined as follow on care from a specific specialist as part of
a specific procedure or service that was performed within the
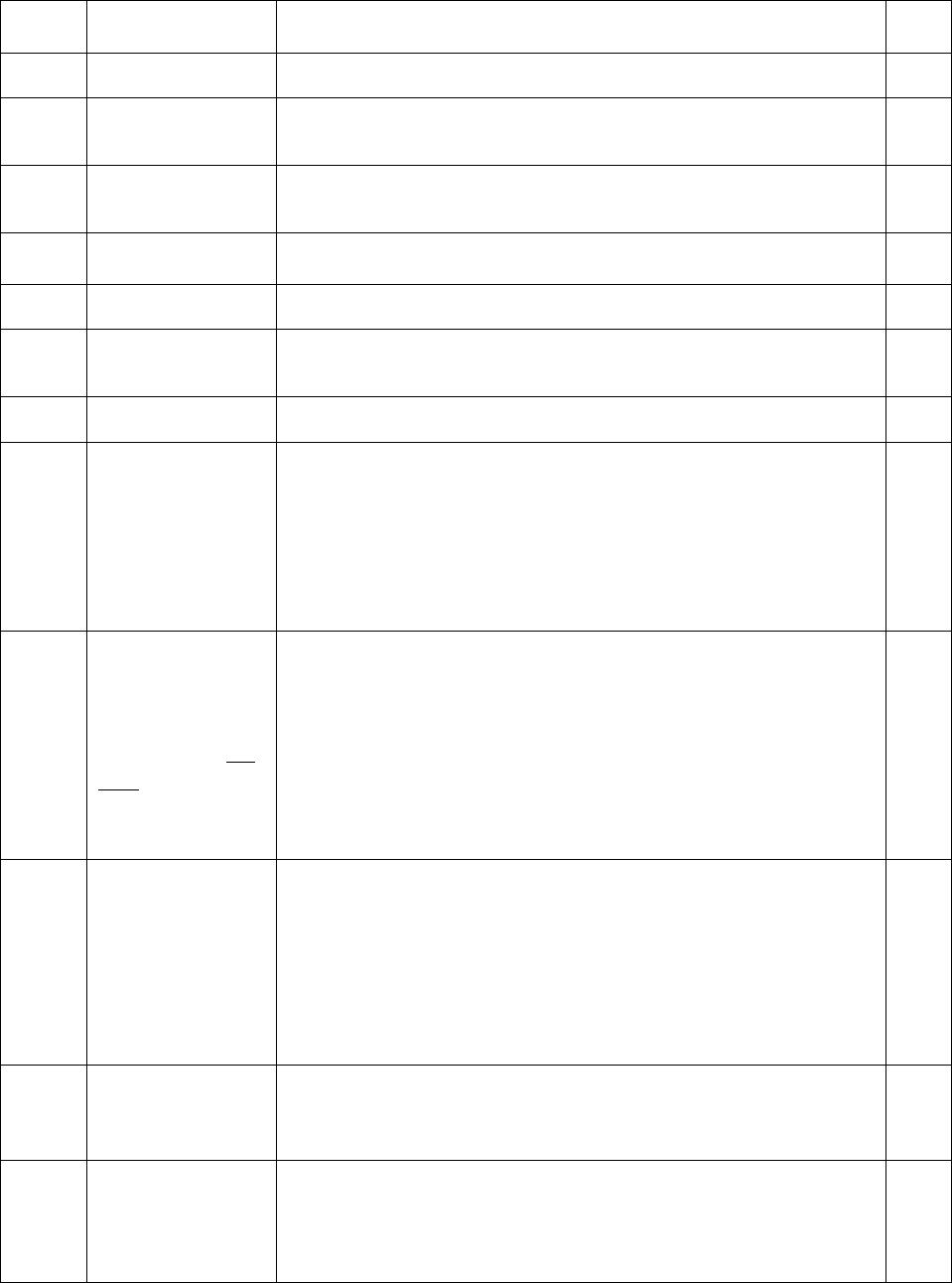
AFI44-176 8 SEPTEMBER 2017 53
No.
Decision Point
Description
Tier
previous six months (TOM, Chapter 8, Section 5)
13.3.4.
[CMD]
Command Directed. Referrals requiring approval from Chief
of the Medical Staff or designee
13.3.5.
[CP]
Capacity. MTF did not have appointments available within
the access to care standards
13.3.6.
[DS]
Distance. Exceeds TRICARE distance/travel requirements
13.3.7.
[NAR]
No Pre-authorization required
13.3.8.
[OHI]
Other Health Insurance. Patient has OHI or is Medicare
eligible
13.3.9.
[POS]
Point of Service or Self-Referred care
13.4.
Laboratory and
Radiology
Orders, DME
Which Require
MCSC
Authorization
The RMC will process and track laboratory and radiologic
orders and Durable Medical Equipment (DME) referrals that
require MCSC authorizations. DME invoices are considered
a “clear and legible report (CLR).”
T-1
13.5.
Laboratory and,
Radiology
Orders,
DME Which Do
Not Require
MCSC
Authorization
If the MTF enters referrals for ancillary services not
requiring MCSC authorizations for electronic tracking
purposes, the MTF will designate the appropriate department
(e.g., radiology, laboratory, medical management, etc.) to
track these “referrals.” This function is not within the scope
of the central RM contract. DME that do not require
authorization is optional.
T-1
13.6.
Disease
Management,
HEDIS
Screening
Preventive care testing does not require TRICARE
authorization; therefore, the RMC will not process, manage,
or track orders/referrals for screening exams. The RMC will
not enter cancer screenings (breast, cervical and colorectal
cancer screenings), HgbA1c results, and LDL HEDIS results
in the TSWF MHSPHP AIM form. This function is not
within the scope of the central RM contract.
T-1
13.7.
Patient Travel
For authorized care outside of the 100 mile MTF-radius, the
TOPA travel section will assist patients with travel
arrangements (Refer to AFI 41-210).
T-1
14.
Right of First
Refusal
Referrals
(ROFRs)
A ROFR is a referral from a beneficiary enrolled to a network
civilian PCM sent to the MTF by the MCSC for appointing
consideration. MTFs should ensure the fullest extent of
ROFR acceptance to sustain clinical currency.
54 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
14.1.
Accept or
Decline ROFRs
The MTF will accept/decline urgent priority ROFRs received
within 90 minutes of receipt or as updated in TOM 8.5. The
MTF will accept/decline routine priority ROFRs received
within two business day of receipt or as updated in TOM
8.5. Failure to respond to ROFR requests within the
prescribed time is an implied MTF declination and the MCSC
will send the patient to the network.
T-0
14.2.
Enter ROFRs in
the EHR
If the ROFR is accepted, the RMC will enter the ROFR into
the EHR as a consult. If the ROFR is entered in CHCS
Referral Booking, convert the referral to a consult in CHCS in
order to track results. In both cases, use the CHCS downtown
provider or generic downtown provider as the referring
provider. Follow MHS GENESIS processes for entering
referrals.
T-0
14.3.
Appoint ROFRs
The RMC or specialty clinic will contact the patients and
schedule their MTF specialty care appointments. See BR 10.
T-0
14.4.
Send ROFR
Referral Reports
to Civilian PCM
The RMC will forward the specialty care report via a HIPAA-
compliant method to the referring civilian PCM within 10-
business days of the patient’s kept appointment.
T-0
15.
Referrals for
Certain Patient
Categories and
Situations
The MTF shall have processes to address the below patient
situations:
T-1
15.1.
ADSM on
Medical Hold
Health Affairs policy 03-026, requires MTFs to ensure
specialty care services are available for ADSMs on “medical
hold” within two weeks of identifying the need for an
appointment. Consult AFI 41-210, TRICARE Operations and
Patient Administration Functions, for specific medical hold
requirements. MTFs should collaborate with their MCSCs to
ensure that ADSMs receive their referral authorizations and
appointments expeditiously. Referring MTF providers will
specify in the body of the referral when the ADSM should
be seen (e.g., 72 hours, 7 days, 14 days, etc.) rather than
using the default 28-day ATC standard for “Routine” priority
referrals.
T-0
15.2.
ADSMs on
Terminal Leave
During the terminal leave period, an ADSM in need of
urgent private sector care must receive a referral and
authorization from his or her MTF Primary Care Manager
(PCM) located at the ADSM’s final duty station. Routine
private sector medical care is authorized only as part of the
ADSM’s active healthcare needs and should be pre-planned
T-0
AFI44-176 8 SEPTEMBER 2017 55
No.
Decision Point
Description
Tier
and pre-authorized collaboratively by ADSM with his or her
PCM. ADSMs on terminal leave may receive routine or
urgent care at a VA medical facility. If an ADSM intends,
while in terminal leave status, to reside outside of the Prime
Service Area of the MTF where the ADSM is enrolled,
utilizing procedures specified in TOM Chapter 17, Section 1,
the MTF shall issue to the MCSC a single preauthorization
for the ADSM to obtain from VA any necessary routine or
urgent outpatient medical care. The period covered by this
preauthorization shall be the entire anticipated span of the
terminal leave period. This preauthorization shall be sent to
MCSC before the ADSM departs his or her final duty station
to commence terminal leave. It shall not include
authorization for any private sector care or specialty care.
ADSMs enrolled overseas traveling or returning stateside
while on terminal leave should contact the OCONUS MCSC
for private sector care authorizations.
Refer to HA Policy “Enrollment of Active Duty Service
Members in Terminal Leave Status” 20120514; HA Policy,
“Policy Memorandum for Preauthorization of Routine and
Urgent Medical Care Provided by the Department of
Veterans Affairs to Active Duty Service Members in
Terminal Leave Status” 20090116.
15.3.
ADSMs and the
Integrated
Disability
Evaluation
System (IDES)
The Physical Evaluation Board Liaison Officer shall work
with the RMC to process referrals for Compensation and
Pension (C&P) examinations at the DVA. The RMC will
ensure the administrative documentation required for C&P
referrals per TOM, Chapter 8.5 are completed prior to
transmitting to the MCSC.
T-0
15.4
ADSM to an
Advanced
Rehabilitation
Center (ARC)
ADSM amputee patients will be referred to DoD ARCs for
assessment before authorizing care in the purchased care.
See ASD(HA) memorandum, 14 Dec 16, Referral of ADSMs
to an ARC.
T-0
15.4.
Prime Patients
with OHI
Other health insurance (OHI) is insurance acquired through
an employer, entitlement program or other source. The RMC
will instruct Prime beneficiaries with OHI to submit referral
requests to their primary health insurer and follow the
guidance provided by their primary health insurer for referral
appointments. Under federal law, TRICARE is the secondary
payer to all health benefits and insurance plans, except for
Medicaid, TRICARE supplements, the Indian Health Service
or other programs or plans as identified by the Defense
T-0
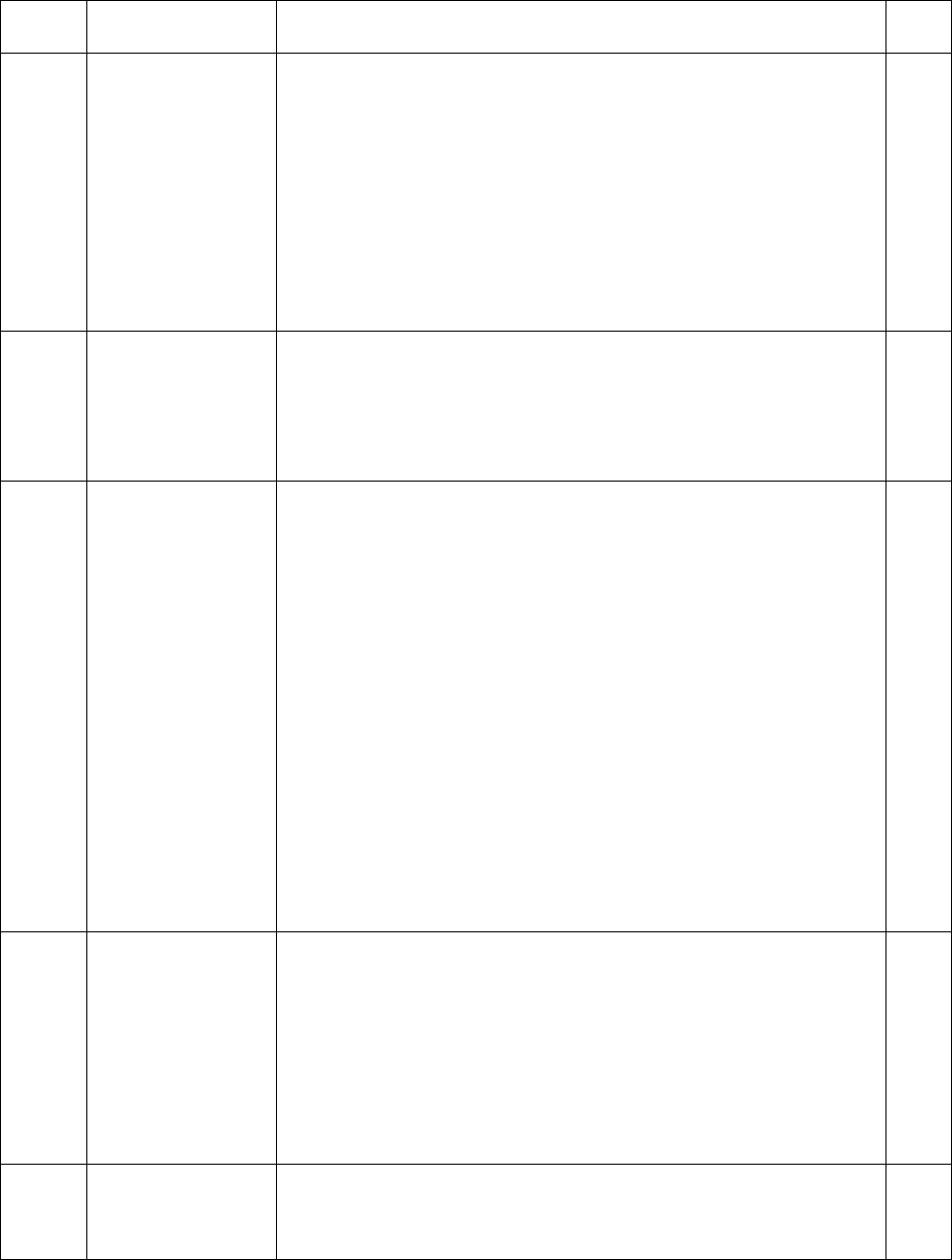
56 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
Health Agency. Request patients to contact the RMC with the
specialist contact information to obtain the CLR.
15.5.
OCONUS Pay
Patients
"Pay Patients" are prioritized for care after ADSMs, Prime
AD Family Members, Prime Retirees/Family members, AF
Family Members not enrolled in TRICARE Prime, and T-
Plus enrollees. "Pay Patients" are eligible to be seen within
the MTF if capacity exists.
15.6.
TRICARE
Plus, TRICARE
For Life (TFL),
Medicare
Beneficiaries
If MTFs have specialty capability and capacity, MTFs are
highly encouraged to accept self-referral specialty care
requests from TFL/Medicare beneficiaries with or without a
referral/request from their civilian PCMs. These
beneficiaries should be afforded the opportunity to be seen in
the MTF based on the MTF’s capability and capacity and
currency case needs. Depending on where the patient
presents, the specialty clinic or the RMC will enter a consult
in CHCS. Obtain civilian physician information from
patient and notate it on the referral. Note: specialty access for
TFL/T Plus patients cannot be at the expense of access for
Prime patients seeking the same specialty care. Prime patients
cannot be deferred to network due to lack of access used by
TFL/T-Plus patients. The RMC will provide the referring
civilian provider/PCM the results within 10 business days
from the kept appointment.
16.
Referral
Tracking
The RMC will track all initial specialty care referral results
generated by the MTF, regardless of beneficiary status or
enrollment, from the time the referral is written until the
results are available to the referring provider or cancelled/not
used by the patient. Referrals generated for tracking purposes
(e.g., labs, radiology, case management, HEDIS, etc.) do not
meet the definition of a specialty care referral/consult and
will not be tracked by the RMC (BRs 4, 13.5).
T-1
17.
Direct Care
Referral Results
If there is a kept MTF appointment associated with the direct
care referral, the referral is considered “closed” and no
further action by the RMC is required. (Note: The referring
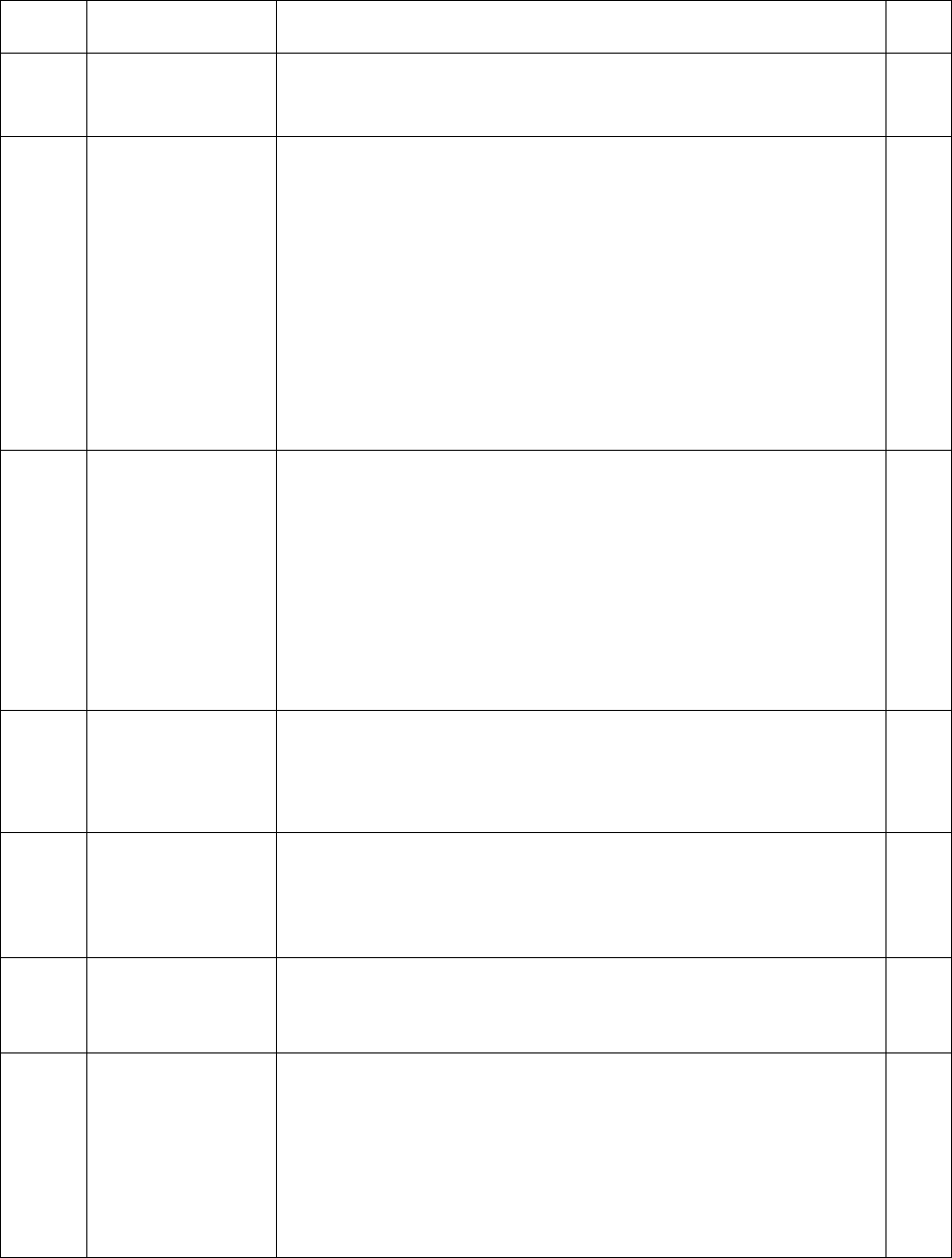
AFI44-176 8 SEPTEMBER 2017 57
No.
Decision Point
Description
Tier
provider should use AHLTA Consult Log to identify which
direct care referrals have a specialist report available for
review.)
18.
ROFR Referral
Results
The RMC will check the status of all accepted ROFRs no
later than 60 days from receipt of the accepted ROFR. If
there is a kept appointment associated with the ROFR, the
RMC will provide the specialty care referral report to the
referring purchased care provider within 10 business days of
the kept specialty encounter. If the patient did not utilize the
referral or keep the appointment, the RMC will close the
referral in CHCS no later than 180 days from the date of
acceptance and annotate {NU} in soft brackets in the CHCS
Review Comment field to indicate the patient did not use the
referral. Notify the referring network provider.
T-0
19.
Purchased Care
Referral Results
The RMC will be the MTF’s single POC to receive all
purchased care CLRs. The RMC will obtain the initial CLR.
Although the RMC does not actively seek CLRs for follow-
up visit, the RMC will provide follow-up CLRs, if received,
to the referring provider. If follow-up visit results are
received from the specialist, the RMC will upload results
into the Health Artifact and Image Management Solution
(HAIMS) and notify the referring provider with a T-CON per
BR 31.
T-1
20.
CLR Received
The RMC/MTF will import CLRs into HAIMS (see BR 32)
and will close the referral in CHCS with a “Deferred Results
Received” (Code #23) status. The RMC will notify the
referring provider of CLRs via T-Con per BR 31.
T-1
21.
When to Start
“Chasing”
CLRs
The RMC will initiate efforts to obtain the CLR as soon as a
claim is discovered, upon request by the referring provider or
no later than 60 days from the date the referral was ordered,
whichever occurs first.
T-0
21.1.
60-Day Mark
When a CLR has not been received or documented in the
EHR, the RMC will check the applicable claims database for
a claim.
T-0
21.2.
Claim
If a claim is found, the RMC will request the CLR from the
rendering purchased care provider. If there is no response
from the provider within 10 calendar days, repeat. If the
provider still does not provide the CLR, the RMC will close
the referral in CHCS using the status of “Deferred results
received” and annotate {CRNRR} in soft brackets in the
CHCS Review Comment Field indicating a claim was
T-0
58 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
reported but no results were received. Notify the referring
provider. Initiate TRICARE contractor procedures as per the
TOM and/or the Memorandum of Understanding (MOU)
with the TRICARE regional contractor. Additionally,
forward a report to the TRICARE Regional Office each
month that lists all provider names, specialty care rendered,
and referral Unique Identifier Numbers for which no CLR
has been received after two attempts or per MOU.
21.3.
No Claim
If no claim is found, the MTF should allow the patient more
time to use referral. MTFs should understand their purchased
care market’s ATC environment.
22.
NLT 180 days
NLT 180 days from the date referral was ordered, if the CLR
has not been received, the RMC will recheck the applicable
claims database for a claim. If there is a claim, follow BR
21.2).
T-0
22.1.
Claim
Follow BR 21.2 above.
T-0
22.2.
No Claim
If there is no claim and the MTF has reminded the patient to
use the referral per BRs 10.4 and 13.2 above, the RMC will
close the referral in CHCS. The MTF will use the below
mandatory closed reason codes in CHCS; use of the other
codes is optional. MTFs on MHS GENESIS will follow
MHS GENESIS processes. The RMC will use only one code
per referral.
T-1
22.2.1.
{NU}
The RMC will close the referral in CHCS with the status of
“No appointment required” (code #13) and will type ‘{NU}”
for “Not Utilized” in the “Review Comment” field
(Mandatory).
T-1
22.2.2.
{CRNRR}
RMC will close the referral in CHCS with the status of
“Deferred Results Received (code #23) and will type
[CRNRR} for “Claim Received No Results Received” in the
“Review Comment” field (Mandatory).
T-1
22.2.3.
{ACPC}
Patient Cancelled via Audio Communicator Referral
Reminder
22.2.4.
{PCRMO}
Patient called the RMC/RMO to cancel the
referral (not via AudioCommunicator
Referral Reminder)
AFI44-176 8 SEPTEMBER 2017 59
No.
Decision Point
Description
Tier
23.
Patient “No
Shows”
The RMC should follow the MTF’s No Show Policy. Define
process when to close the referral (e.g., after 1, 2, or 3 ‘No
Shows” and who will close the referral in CHCS (e.g., the
specialty clinic who documented the “No Show,” the RMC,
or the referring provider/clinical team).
24.
Notify
Providers of
Unused,
Cancelled,
Denied
Referrals
The RMC will notify the referring provider of all routine
priority referrals not used or cancelled by their patients IAW
local MTF policy, but no less than monthly. (Note: the RMC
should utilize RMS to generate a report by referring provider
for the desired date range and provide it to leadership IAW
local MTF policy.)
T-1
25.
STAT / Urgent
Referral Results
If immediate results for STAT and urgent priority specialty
care referrals are clinically required, then the PCM/clinical
team should request them from the purchased care specialist.
The clinic should provide the purchased care provider the
RMC fax number. If the PCM/clinical team need the referral
results for a future scheduled patient appointment regarding
the CLR results, and the CLR results are not in AHLTA,
HAIMS or the medical records, then the PCM/clinical team
should provide the RMC as much prior notice as possible for
the RMC to obtain the needed CLR.
26.
Automatic
CHCS Closure
of Referrals
MTFs will disable the automatic closure function in CHCS
for referrals/consults.
T-1
27.
Import CLRS
into the EHR
The RMC shall import the following documents into the
EHR within three working days from receipt of results: the
initial specialty care CLR; follow-up CLRs; urgent primary
care results; and laboratory results and radiology reports that
require an authorization. All other loose documents shall be
imported into HAIMS by Medical Records per AFI 41-210.
MTFs using MHS GENESIS will upload the CLR into MHS
GENESIS. Non-MHS GENESIS MTFs will upload the CLR
into HAIMS.
T-1
28.
MHS GENESIS
MTFs
The RMC should follow procedures for importing documents
into MHS GENESIS and provider notification.
29.
Non-MHS
GENESIS
MTFs
The MTF will create a T-Con and HAIMS entry for each
CLR/result.
The MTF will associate the T-Con with the HAIMS entry so
that the reviewing provider clearly understands which T-Con
is for which HAIMS entry.
T-1
60 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
For both parts, the MTF will use the following mandatory
standard naming convention: Network Results – Specialty
MM/DD/YY where the MM/DD/YY is the date the patient
was seen. For example, Network Results – Cardiology
2/10/14.
If the local HAIMS is down, the MTF will select alternative
Healthcare Artifact and Image Repository (HAIR) to upload
CLRs and include the link to the alternative HAIR in the
provider notification T-Con.
29.1.
Shared Folders in
Shared Drives
The MTF shall not maintain any existing shared folders used
for the purpose of storing temporary results or other
Protected Health Information longer than 30 calendar days
following the date of the original image upload. Thereafter,
the electronic folder and documents must be deleted (AFI 41-
210)
T-1
29.2.
Original and
Translated CLRs
(OCONUS)
The MTF shall import both the original foreign language and
the English translated CLR into HAIMS. The untranslated
result/CLR does not have to be signed by the referring
provider if the translated result/CLR was already signed.
T-1
29.3.
Wet Signatures;
Hard Copy of
Referral
Once loaded into HAIMS, the reviewing provider is not
required to handwrite or “wet” sign the hard copy
result/report. The paper copy of the result/report is not
required to be filed into the paper outpatient medical record.
However wet signatures and filing of paper copy may be
required for special programs (e.g. PRP) or payment issues).
Before destroying the original hard copy or electronic
result/report, ensure that the scanned document is legible by
the provider. Ensure you have a quality check process in
place to ensure right patient, right CLR and right record.
Correcting errors: The MTF will have a quality check process
to minimize PHI/PII errors.
30.
Create HAIMS
Encounter
The MTF will create a HAIMS encounter for the CLR. See
HAIMS RM Workflow Training slides_Nov 2013_Colorado
MSMO found at AFMS Knowledge Exchange.
T-1
31.
Create AHLTA
T-Con
The MTF will follow the below process:
Under the Folder List, select “Telephone Consults.”
From the Toolbar/Action bar, click “New Telcon” icon; click
“Yes” in the pop-up.
In the “Clinic” field, select the clinic location of the provider
T-1
AFI44-176 8 SEPTEMBER 2017 61
No.
Decision Point
Description
Tier
receiving the T-Con. AHLTA automatically defaults this
field to the creator’s location. You must change it. Once
you click “OK,” you cannot make changes. If you chose the
wrong clinic and clicked “OK”, you must cancel the T-Con
and start over.
In the “Assigned Owner” field, select the provider receiving
the T- Con.
In the “Reason for Telephone Consult” field, enter the
following mandatory naming convention: “Network Results
– Specialty MM/DD/YY”.
For example, “Network Results – Orthopedics 02/13/14”
or “Network Results – Lab 02/13/14”; or “Network Results
– Radiology 02/04/14”.
The entry should match the name of the corresponding
HAIMS entry
Click “OK” when done. Your T-Con will automatically
display.
If sending a courtesy copy notification of a result/report, use
the following naming convention: “Network Results -
Specialty MM/DD/YY—CC” (CC=courtesy copy).
In the “Note” field, reference the HAIMS entry in the T-Con.
For example, “Please review the results in HAIMS titled
Network Results – Orthopedics 02/13/14”. For T-Con:
In the “Note” field, enter text. For example, “Please review
the results in HAIMS titled Network Results – Orthopedics
2/13/14”.
In the “Urgency” field, AHLTA defaults to “Medium.”
Change as appropriate.
In the “Diagnosis” box, select “Z76.89 - Persons
encountering health services in other specified
circumstances”.
In the “Admin” box:
In the “Meets Output Visit Criteria (Workload)?” field,
change the default “Yes” to “No”.
In the “E & M” field, ensure “99499” is selected.
From the Toolbar/Action bar, click “Save” and “Close”
icons. Do not sign the T-Con. The receiving provider will
62 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
sign the T-Con. The T-Con is automatically sent to the
selected provider.
32.
Upload CLR in
HAIMS and
Associate
T-CON
The MTF will follow the below process:
From the Folder List, select Artifacts and Images. (Note:
Telecon Tab is still open).
Select Import Asset icon
In the “Acquire Asset Import New” box, ensure “Browse and
upload a file” and “Associate with Selected Encounter”
boxes are checked.
Select “Browse” and locate CLR. Click “Upload”
Fill in Metadata fields as instructed in BR 33.5.
Select “Save and Close”
Close Artifacts and Images screen. Select “Close” button on
toolbar. CLR is now available in HAIMS and is associated
with the T-CON created, which makes it easier for the
provider to find the HAIMS CLR.
T-1
32.1.
Mandatory
HAIMS
Metadata Fields
The MTF will fill out the below mandatory HAIMS metadata
fields for CLRs:
Author Name: The author name is the purchased care
provider or group that provided the CLR.
Date Document Created: The date that the patient visit
occurred or the date of the CLR. (For mental health CLRs,
check box titled, “Mark as Sensitive.”)
Document Type: Use the dropdown menu: for CLRs, select:
Encounter Note—Consultation. Others, Radiologic report,
Procedure Note, etc.
Document Title: Network Results – Specialty MM/DD/YY
where the date is the date in #2 above.
Save and Close
T-1
32.2.
Optional
Metadata Fields
Practice Setting: Outpatient
Specialty: Type a few characters and choose (e.g.
orthopedics)
Procedure or Service: type a few characters and choose (e.g.,
MRI)
AFI44-176 8 SEPTEMBER 2017 63
No.
Decision Point
Description
Tier
Save and Close
33.
Provider
Review
At a minimum, providers will document their review of the
HAIMS CLR in the corresponding T-Con. Ensure T-Con is
non-count workload. Change T-Con medical coding as
appropriate. Sign and close.
Providers will review T-Cons notifying them of scanned
results/reports within three business days from the receipt of
the T-Con. Providers will have current surrogates in
CHCS/AHLTA to review T-Cons in their absence.
Completed T-Cons are assumed to mean that the provider has
reviewed the result/report in HAIMS/AHLTA.
T-1
34.
CHCS Ad Hoc
to Monitor
Provider
Review of
Scanned CLRs
When the T-Con naming convention is used per policy
instructions, MTFs may use the CHCS Provider Review Ad
Hoc that displays which CLRs had been scanned into
HAIMS and whether or not they have been reviewed. These
can be identified by patient or by provider.
On the printed ad hoc report, if theT-Con has been reviewed,
a status of “Tel-Con status” will show next to the T-Con. If
the T-Con has NOT been reviewed, a status of “Occ-Svc
status” will show next to the T-Con.
35.
Measures
The MTF will report the below measures to MTF Executive
leadership at least quarterly. Items 1-5 can be obtained from
Referral Mgt Performance Mgt Tool (RMPMT). Items 8-9
can be obtained in RMS.
1. Number of specialty care referrals/consults
2. Number of urgent primary care referrals
3. Number of referrals seen in the MTF or to other MTFs
4. Number of referrals deferred to the purchased care
5. Number and percentage of ROFRs accepted from the
MCSC (Note: if the MTF has no ROFR capability, then
items 5 and 6 are N/A)
6. Percent ROFR referral results sent to requesting civilian
PCM within 10 days of the kept appointment
7. Number and percent of initial specialty referrals that were
dispositioned within one business day as “Appoint to the
MTF” or “Defer to Network.
CLR Percent Received Report
T-2
64 AFI44-176 8 SEPTEMBER 2017
No.
Decision Point
Description
Tier
36.
Secure
Messaging
(SM), MiCare
The RMC should check their assigned SM box several times
a day for new messages. The RMC should use SM to answer
patient questions on referrals, obtain results from purchased
care providers who are using the same SM vendor, and
communicate with providers/clinical teams. Using SM to
communicate with patients and purchased care providers
about referrals saves the RMC time by decreasing
unnecessary phone calls and eliminating telephone tag.
AFI44-176 8 SEPTEMBER 2017 65
Attachment 3 (Added)
ACCESS MANAGEMENT TEAM (AMT) AGENDA
Chair: Group Practice Manager (GPM)
Alternate Chair: Chief of the Medical Staff (SGH)
Required Attendees: Access Manager, all GPMs, Chief of Medical Staff (SGH), Chief Nurse
(SGN), Chief Administrator (SGA); Health Care Integrator (HCI); Health Service
Management 4A0 Functional representative; Aerospace Medicine Chief (SGP) or
Representative; Flight Commanders of all clinics, TRICARE Operations and Patient
Administration (TOPA) Flight Commander, the Quality Manager, and the lead appointment
agent.
Frequency: Meet in-person with AMT members listed above (IAW AFI 44-176 para 2.2.2) at
least monthly.
Standard Agenda items will include but are not limited to:
1) Review and coordination of: templating, scheduling, appointing, clinic/appointment staffing,
provider coverage, supply shortfalls and surpluses, clinical operational issues with the goal of
optimizing ATC at the MTF, process improvement efforts.
2) Review performance measures for all clinics monthly, to include, but not limited to:
a) Third Next available appointment (24HR, FTR, SPEC)
b) Appointment Utilization
c) Demand Management
d) Purchased care leakage
e) Patient satisfaction
f) Telephony metrics
g) No-show metrics
h) First call resolution results
i) PCM Continuity measures
j) NAL metrics (e.g., updates, NAL booking analysis metric, warm-handoff metric,
beneficiaries pre-intent versus NAL recommended disposition metrics)
k) Minimum of 180-calendar days of available appointments for booking at all
times for specialty and primary care clinics.
AMT Meeting Documentation: Evidence of AMT meeting occurrence (i.e. slides and sign-in
roster) must be documented. Formal meeting minutes are encouraged but not required.
